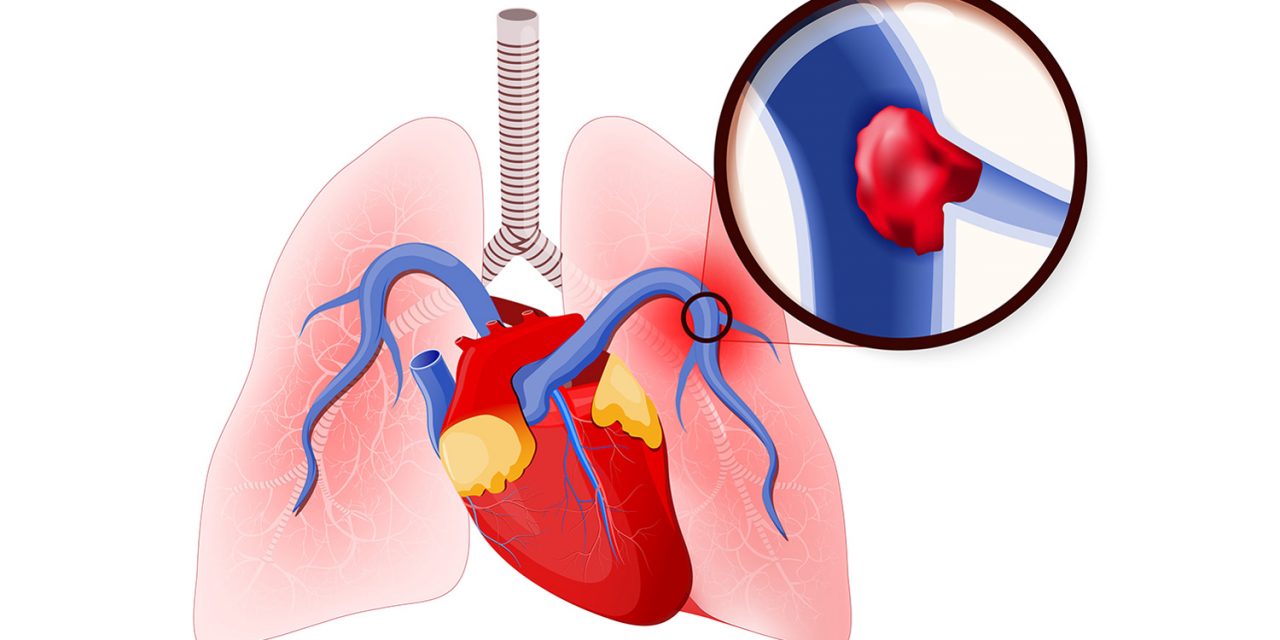
A pulmonary embolism is a blockage in the pulmonary artery, which supplies the blood to the lungs. It is one of the most common cardiovascular diseases.
Pulmonary embolism affects about 1 in 1,000 people every year in India. The obstruction, usually a blood clot, prevents oxygen from reaching the lung tissue. This means that it can be fatal. The word “embolism” comes from the Greek émbolos, meaning “stopper” or “plug.” In a pulmonary embolism, the embolus is formed in one part of the body, the whole. The blood supply seeps into it, and then it stops blood flow through the lungs to another part of the body. An embolus is different from a thrombus, which forms and stays in one place.
Symptoms
Symptoms of pulmonary embolism include:
- Chest pain, a sharp, stabbing pain that might become worse when breathing increased or irregular heartbeat
- Dizziness
- Difficulty catching breath, which may develop either suddenly or overtime
- Rapid breathing
- A cough, normally dry but possibly with blood, or blood and mucus.
Causes
A pulmonary embolism occurs when an embolus, usually a blood clot, blocks the blood flow through an artery that feeds the lungs. A blood clot may begin in an arm or leg. Known as deep venous thrombosis (DVT). After that, it is freed and travels through the circulatory system towards the lungs. There, the passage through small vessels is very large, so it creates a blockage. This blockage prevents blood from flowing to one part of the lung. This causes the affected part of the lung to die due to a lack of oxygen. Rarely, a pulmonary embolism may arise from an embolus that is formed from droplets of fat, amniotic fluid, or some other particle that enters the bloodstream.
Treatment
The first step in the treatment of most embolism is to provide shock treatment and oxygen therapy. Anticoagulant drugs, such as heparin, enoxaparin, or warfarin, are usually given to thin the blood and prevent further clotting. Required, they should be treated with an anticoagulant management service, not their primary care physician. Drug clots called ticks-break can also be administered. However, they carry the risk of excessive bleeding. Thrombolytics include actives, retavas, and aminase. If the patient has low blood pressure, dopamine can be given to increase the pressure. The patient will usually have to take medication regularly for an indefinite amount of time, usually at least 3 months.
Prevention
A number of measures can reduce the risk of a pulmonary embolism.
A high-risk patient may use anticoagulant drugs such as heparin or warfarin.
Compression of the legs is possible, using anti-embolism compression stockings or pneumatic compression. An inflatable sleeve, glove, or boot holds the affected area and increases the pressure when required.
Compression methods prevent blood clots by accumulating blood in the deep veins and reducing the amount of blood that has accumulated. Other methods of reducing risk include physical activity, regular exercise, a healthy diet, and quitting smoking or tobacco consumption.
Diagnosis
To reach a diagnosis, the doctor will look at the patient’s history and consider whether an embolism is likely. They will carry out a physical examination. Diagnosis can be challenging because other conditions have similar symptoms.
Tests for diagnosing pulmonary embolism include:
- A mathematical model that helps a doctor predict the course of DVT and the risk of an embolism
- D-Dimer test, a blood test that can diagnose thrombosis that can rule out further testing if it produces a negative result
- Pulmonary V/Q scan, two tests that analyze the ventilation and structural properties of the lungs and give off less radiation than a CT
- Computerized tomography (CT) scan, which can reveal abnormalities in the chest, brain, and other organs, and in cases where a V/Q is not possible
- Electrocardiogram (EKG), to record the electrical activity of the heart
- Arterial blood gas study, to measure oxygen, carbon dioxide, and other gases in the blood
- Chest X-rays, to generate a picture of the heart, lungs, and other internal organs
- Ultrasound of the legs, to measure the speed of blood flow velocity and any changes
- Pulmonary angiogram, to reveal blood clots in the lungs
- Magnetic resonance imaging (MRI), to obtain detailed pictures of internal structures.
Risk Factors
The risk of developing pulmonary embolism increases with age. People who have conditions or diseases that increase the risk of blood clots are more likely to develop a pulmonary embolism. A person is at greater risk of a pulmonary embolism if they have a leg or arm (DVT). ) Have a blood clot, or if they have had a pulmonary embolism in the past. Prolonged bed rest or inactivity increases the risk of DVT and therefore A, there is an increased risk of pulmonary embolism. It can be a long flight or a car ride. When we don’t move much, our blood accumulates in the lower parts of our body. If the blood is circulating less than normal, the blood clot is more likely to form. Damaged blood vessels also increase the risk. This may be due to injury or surgery. If a blood vessel is damaged, the blood vessel can become narrower, increasing the chances of blood clots forming. Other factor risks include some cancers, inflammatory bowel disease, obesity, pacemakers, intravenous catheters, pregnancy, Estrogen supplements, family history of blood clots and smoking.
2,674 Comments
zprГЎvy
flibanserin 0.3mg
Great post. I was checking continuously this weblog and I’m inspired! Very useful info particularly the closing part 🙂 I care for such info much. I was looking for this particular info for a very long time. Thank you and best of luck.
nimotop
Hello dratulkasliwal.in webmaster, Keep the good content coming!
luvox medication
indocin 10mg
tato strГЎnka
Great, thanks for sharing this blog post.Really looking forward to read more. Really Great.
allopurinol 300 mg pharmacy
To the dratulkasliwal.in webmaster, You always provide helpful information.
amaryl 40mg
doxycycline 100mg
floxin 20mg
To the dratulkasliwal.in owner, Excellent work!
aristocort 150mg
speciell info
What is Alpha Tonic? Alpha Tonic stands as a natural health supplement designed to comprehensively address men’s overall well-being.
mais informações aqui
FitSpresso is a natural weight loss supplement that will help you maintain healthy body weight without having to deprive your body of your favorite food or take up exhausting workout routines.
aciphex 100mg
Very interesting details you have mentioned, thankyou for putting up.
An interesting discussion is worth comment. I think that you should write more on this topic, it might not be a taboo subject but generally people are not enough to speak on such topics. To the next. Cheers
coreg 60mg
pepcid 100mg
meer informatie
You could definitely see your expertise in the paintings you write. The sector hopes for more passionate writers such as you who aren’t afraid to say how they believe. At all times go after your heart.
fonte
Super-Duper site! I am loving it!! Will be back later to read some more. I am taking your feeds also
I’d must test with you here. Which is not something I normally do! I get pleasure from reading a submit that can make folks think. Additionally, thanks for allowing me to remark!
I dugg some of you post as I cogitated they were very useful handy
There is obviously a bundle to know about this. I consider you made certain nice points in features also.
Thanks a bunch for sharing this with all of us you actually understand what you are talking approximately! Bookmarked. Please also talk over with my web site =). We may have a hyperlink exchange contract between us!
Hello dratulkasliwal.in admin, Your posts are always a great source of information.
pulmicort 200mСЃg pharmacy
napsauta resursseja
Just desire to say your article is as surprising. The clarity for your submit is just excellent and i could assume you’re an expert in this subject. Well along with your permission let me to snatch your RSS feed to stay updated with forthcoming post. Thank you a million and please carry on the enjoyable work.
Nagano Lean Body Tonic: An IntroductionNagano Lean Body Tonic is a dietary supplement designed to help lose unhealthy weight.
WONDERFUL Post.thanks for share..more wait .. …
casodex 20mg
I’ve been absent for a while, but now I remember why I used to love this blog. Thank you, I will try and check back more frequently. How frequently you update your site?
I liked as much as you will obtain performed right here. The comic strip is attractive, your authored subject matter stylish. however, you command get bought an nervousness over that you would like be handing over the following. ill without a doubt come more until now once more since exactly the similar nearly a lot incessantly within case you protect this hike.
tu peux vГ©rifier ici
Good day! Do you know if they make any plugins to safeguard against hackers? I’m kinda paranoid about losing everything I’ve worked hard on. Any recommendations?
I think other website proprietors should take this website as an example , very clean and fantastic user friendly layout.
Hi dratulkasliwal.in webmaster, Thanks for the well-presented post!
To the dratulkasliwal.in webmaster, Your posts are always well-balanced and objective.
Hello dratulkasliwal.in owner, Your posts are always well-cited and reliable.
Dear dratulkasliwal.in owner, Thanks for the in-depth post!
excellent post, very informative. I’m wondering why the opposite specialists of this sector don’t notice this. You must continue your writing. I am confident, you’ve a huge readers’ base already!
prevacid 40mg
Hi dratulkasliwal.in webmaster, Thanks for the well-researched and well-written post!
Hello dratulkasliwal.in administrator, You always provide in-depth analysis and understanding.
Hi dratulkasliwal.in webmaster, Thanks for the well-organized post!
Hi dratulkasliwal.in administrator, Your posts are always a great source of knowledge.
Hi dratulkasliwal.in admin, You always provide great insights.
To the dratulkasliwal.in owner, Thanks for the in-depth post!
alesse 10mg
To the dratulkasliwal.in administrator, Thanks for the in-depth post!
wellbutrin 25mg
Very interesting information!Perfect just what I was looking for!
Hi dratulkasliwal.in webmaster, Keep sharing your knowledge!
You made a number of fine points there. I did a search on the theme and found mainly folks will agree with your blog.
clonidine 0,1mg without a doctor prescription
FitSpresso is a natural weight loss supplement crafted from organic ingredients, offering a safe and side effect-free solution for reducing body weight.
Hello dratulkasliwal.in admin, Your posts are always well thought out.
acesse este site
It’s really a nice and useful piece of info. I’m glad that you shared this useful information with us. Please keep us up to date like this. Thank you for sharing.
dostinex 50mcg
tofranil 25mg
Great – I should definitely pronounce, impressed with your web site. I had no trouble navigating through all tabs and related info ended up being truly simple to do to access. I recently found what I hoped for before you know it at all. Reasonably unusual. Is likely to appreciate it for those who add forums or anything, site theme . a tones way for your client to communicate. Excellent task..
About Blue Tonic Weight Loss Drink Recipe:The Blue Tonic Weight Loss Drink Recipe is more than just a beverage; it’s a potent blend of carefully selected ingredients designed to support your weight loss journey.
彼らの説жЋ
I’m still learning from you, while I’m trying to achieve my goals. I absolutely enjoy reading everything that is written on your blog.Keep the posts coming. I liked it!
I like this blog so much, saved to bookmarks. “American soldiers must be turned into lambs and eating them is tolerated.” by Muammar Qaddafi.
I think this is one of the most significant info for me. And i’m glad reading your article. But should remark on few general things, The site style is perfect, the articles is really excellent : D. Good job, cheers
orlistat 60mg medication
Hello.This article was extremely remarkable, particularly since I was looking for thoughts on this issue last Friday.
Greetings! I know this is kinda off topic but I was wondering which blog platform are you using for this site? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at options for another platform. I would be great if you could point me in the direction of a good platform.
site
Only wanna input on few general things, The website layout is perfect, the written content is really excellent. “By following the concept of ‘one country, two systems,’ you don’t swallow me up nor I you.” by Deng Xiaoping.
speciell info
Hey just wanted to give you a quick heads up. The words in your content seem to be running off the screen in Opera. I’m not sure if this is a formatting issue or something to do with internet browser compatibility but I figured I’d post to let you know. The layout look great though! Hope you get the problem resolved soon. Thanks
I loved as much as you’ll receive carried out right here. The sketch is attractive, your authored material stylish. nonetheless, you command get got an nervousness over that you wish be delivering the following. unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this increase.
Lovely just what I was searching for.Thanks to the author for taking his clock time on this one.
allegra 20mg
I simply could not leave your web site before suggesting that I actually enjoyed the usual information a person provide to your guests? Is gonna be back steadily to investigate cross-check new posts.
Thank you for sharing your info. I truly appreciate your efforts and I am waiting for your next write
ups thank you once again.
katalog
Good blog! I really love how it is simple on my eyes and the data are well written. I am wondering how I might be notified whenever a new post has been made. I’ve subscribed to your feed which must do the trick! Have a nice day!
fГҐ fakta
гЃ“гЃ“г‚’г‚ЇгѓЄгѓѓг‚Ї
Hello dratulkasliwal.in webmaster, Thanks for the well-organized and comprehensive post!
What’s Taking place i am new to this, I stumbled upon this I have found It absolutely useful and it has helped me out loads. I am hoping to give a contribution & help other customers like its helped me. Good job.
Some truly nice and useful information on this web site, besides I conceive the pattern has got wonderful features.
Great – I should certainly pronounce, impressed with your site. I had no trouble navigating through all the tabs as well as related info ended up being truly easy to do to access. I recently found what I hoped for before you know it in the least. Reasonably unusual. Is likely to appreciate it for those who add forums or something, website theme . a tones way for your client to communicate. Excellent task..
Some truly nice stuff on this website , I love it.
I love it when people come together and share opinions, great blog, keep it up.
Thank you ever so for you blog. Really looking forward to read more.
My website: russkoeporno365
Muchos Gracias for your article.Really thank you! Cool.
My website: anilingus.tv
It’s in point of fact a nice and helpful piece of info. I’m happy that you shared this useful information with us. Please keep us informed like this. Thanks for sharing.
Thanks for sharing, this is a fantastic blog post.Really thank you! Much obliged.
My website: анилингус порно
Thanks for sharing, this is a fantastic blog post.Really thank you! Much obliged.
My website: russkoeporno365.pro
You have brought up a very fantastic details, appreciate it for the post.
Thanks-a-mundo for the post.Really thank you! Awesome.
My website: анал порно
Keep functioning ,terrific job!
pentasa 2mg
I just like the helpful info you provide to your articles. I’ll bookmark your weblog and test again right here frequently. I’m somewhat certain I’ll be informed lots of new stuff proper right here! Good luck for the following!
prednisolone 10mg
Thanks-a-mundo for the post.Really thank you! Awesome.
My website: chastnoeporno.top
Hey! I could have sworn I’ve been to this site before but after browsing through some of the post I realized it’s new to me. Anyhow, I’m definitely delighted I found it and I’ll be bookmarking and checking back often!
I am extremely impressed with your writing skills and also with the layout on your blog. Is this a paid theme or did you customize it yourself? Anyway keep up the excellent quality writing, it?s rare to see a great blog like this one these days..
Very good post.Really looking forward to read more. Great.
My website: анальное порно
Woah! I’m really loving the template/theme of this blog. It’s simple, yet effective. A lot of times it’s hard to get that “perfect balance” between superb usability and visual appearance. I must say you’ve done a great job with this. Additionally, the blog loads extremely quick for me on Chrome. Excellent Blog!
I am incessantly thought about this, thanks for posting.
My website: анальное порно
Thanks for sharing, this is a fantastic blog post.Really thank you! Much obliged.
My website: анальное порно
I am not really fantastic with English but I get hold this rattling leisurely to understand.
As a Newbie, I am continuously exploring online for articles that can be of assistance to me.
My website: russkoeporno365.pro
Definitely, what a great blog and revealing posts, I definitely will bookmark your site. Best Regards!
My website: анальное порно
Thanks for sharing, this is a fantastic blog post.Really thank you! Much obliged.
My website: analporno.club
I like the valuable information you provide in your articles. I’ll bookmark your weblog and check again here frequently. I am quite certain I will learn lots of new stuff right here! Good luck for the next!
Thank you for sharing excellent informations. Your web-site is very cool. I am impressed by the details that you’ve on this website. It reveals how nicely you understand this subject. Bookmarked this website page, will come back for extra articles. You, my pal, ROCK! I found simply the info I already searched all over the place and simply couldn’t come across. What a great web-site.
Hey there! Someone in my Myspace group shared this site with us so I came to give it a look. I’m definitely loving the information. I’m book-marking and will be tweeting this to my followers! Wonderful blog and terrific design.
I truly appreciate this post. I¦ve been looking everywhere for this! Thank goodness I found it on Bing. You’ve made my day! Thanks again
Great blog here! Also your web site loads up fast! What host are you using? Can I get your affiliate link to your host? I wish my website loaded up as quickly as yours lol
Together with every little thing which appears to be developing inside this particular subject matter, many of your opinions happen to be somewhat refreshing. However, I appologize, but I can not subscribe to your entire strategy, all be it radical none the less. It seems to us that your comments are not completely justified and in actuality you are your self not really totally certain of your assertion. In any case I did appreciate reading it.
Yeah bookmaking this wasn’t a speculative conclusion outstanding post! .
zestoretic
You are my intake, I have few web logs and very sporadically run out from to post .
Cutest Pornstars: The Good, The Bad, And The Ugly porn Stars
Technology Is Making Popular Casino Slots Better Or Worse?
online casino Slots (taodemo.com)
Have you ever thought about adding a little bit more than just your articles? I mean, what you say is valuable and everything. Nevertheless think about if you added some great visuals or video clips to give your posts more, “pop”! Your content is excellent but with images and clips, this website could definitely be one of the very best in its niche. Fantastic blog!
I went over this site and I believe you have a lot of fantastic information, saved to fav (:.
bactrim 300mg
How To Build A Successful Cleveland Mesothelioma Attorney When You’re Not Business-Savvy mesothelioma attorneys san diego
(May)
Nice post! You have written useful and practical information. Take a look at my web blog Webemail24 I’m sure you’ll find supplementry information about Data Mining you can gain new insights from.
How To Get Better Results Out Of Your Lawyers For Accident injury and accident lawyer (Archer)
Nice post! You have written useful and practical information. Take a look at my web blog Seoranko I’m sure you’ll find supplementry information about Social Bookmarking Sites you can gain new insights from.
A Provocative Remark About Programming Car Key cut and program car key
See What Bmw Spare Key Tricks The Celebs Are Using bmw spare key
10 Ways To Create Your Truck Accident Lawyer Empire
columbus truck accident attorney [Joie]
Bandar Online Togel’s History Of Bandar Online Togel In 10 Milestones
Togel4d
14 Businesses Doing A Superb Job At Bunk Bed Single Double triple bunk bed Single
losartan 100 mg over the counter
Learn The Athens Birth Injury Attorney Tricks The Celebs Are
Making Use Of attorney birth injury pennsylvania (Alfie)
10 Misconceptions Your Boss Holds Concerning Grey Sectional
Sofa Green Sectional Sofa
10 Things We All We Hate About Pull Out Sofa Couch pull out Sectional couch with storage
How To Choose The Right Veleco On The Internet veleco Mobility scooter
24 Hours For Improving Electric Fireplace Suite
UK freestanding Fireplace suites
10 Saab Replacement Key-Related Projects To Extend Your Creativity Workshop
How To Save Money On Folding Treadmill zackfoxworth
The Worst Advice We’ve Ever Received On Symptoms Of Adhd Adults Test high-functioning adhd in females symptoms
The 10 Most Scariest Things About Link Togel link togel
This Is A Treehouse Bunk Bed With Slide Success Story You’ll
Never Believe treehouse Double Bed
Ten Things You Learned In Kindergarden That’ll Help You With Double Pushchair convertible double pushchairs
Go88 la thien duong game bai doi thuong uy tin so 1 Viet Nam. Link trang chu chinh thuc Go88.com, Dang ky nhan thuong +50K. website: https://mkstalin.net/
For anyone who hopes to find valuable information on that topic, right here is the perfect blog I would highly recommend. Feel free to visit my site ZQ3 for additional resources about Cosmetic Treatment.
The Reasons You’ll Want To Find Out More About Bandar Toto
Toto Macau
10 Things Everyone Hates About Nespresso White Machine Nespresso Coffe machines
5 Tools Everyone In The Stoves Retro Fridge Freezer Industry Should Be Making Use Of
slim retro fridge freezer
10 Unexpected Bifold Repairs Near Me Tips bifold doors Repair
Five Killer Quora Answers To Bi Fold Door Repair Near Me
bi fold Door repair near Me
15 Twitter Accounts That Are The Best To Learn More About Railroad Injuries Law
railroad Accident lawyer Near Me portland oregon
The 9 Things Your Parents Taught You About Bifold Repairs Near Me Bifold Repairs Near Me
The No. One Question That Everyone Working In Mesothelioma Lawsuit Payouts Should Know How
To Answer Philadelphia mesothelioma attorneys
15 Lessons Your Boss Wished You’d Known About Medication For
ADHD Adhd Depression Medication
15 Terms That Everyone Working In The Mesothelioma Attorney Industry
Should Know Mesothelioma Claims
This Week’s Most Popular Stories About Windows Repair Windows repairs near me
How To Know If You’re In The Right Place To Go After Lexus Car Key lexus remote
key replacement (wooriwebs.com)
Sunwin cong game doi thuong so 1 Viet Nam. SunWin Club so huu dang tu no hu, ban ca, casino truc tuyen dac biet la sanh game bai hap dan nhat thi truong ca cuoc.
Wedsite: https://sunwin100.club/
nhi xinh dep
nhi https://www.dratulkasliwal.in/blog/tavi-in-cardiology/
5 Killer Quora Answers On Programing Keys transponder key
programmer (question-ksa.com)
medrol
Indisputable Proof Of The Need For Programing Key key programmer (Della)
Are You Getting The Most From Your Reprogramming Car Key?
Reprogram Key Fob
Car Keys Programming 101: This Is The Ultimate Guide For Beginners
car keys programming Near me
Hi there, I simply couldn’t leave your website without saying that I appreciate the information you supply to your visitors. Here’s mine Article Star and I cover the same topic you might want to get some insights about SEO.
An In-Depth Look Into The Future What Is The Programmed
Car Keys Industry Look Like In 10 Years? Car key reprogram near me
Why Program A Car Key Is More Difficult Than You Imagine how to program a car key
Do You Think You’re Suited For Doing Car Key Programer?
Take This Quiz Smart Key Programming Near Me
10 Things That Your Family Taught You About Car Key Fob Programming Near Me car key fob programming near me
Seo Design For Top Search Engine Ranking Over And Over 백링크 확인
78win hay thuong duoc biet den voi 78Win.com la nha cai ca cuoc truc tuyen uy tin hang dau tai Viet Nam va Chau A. Dang ky 78 Win Casino, tai APP choi game bai, no hu, ban ca, tai xiu, xo so, xoc dia…
Website: https://78winsg.asia/
12bet nam trong danh sach dia chi ca cuoc truc tuyen uy tin hang dau hien nay. He thong chinh thuc ra mat thi truong ca cuoc sau khi da co dinh huong ro rang ve chien thuat phat trien. Sau nhieu nam hoat dong, thuong hieu ke tren hien phat trien he thong ve tinh rong khap Chau A. http://12betsg.asia/
10 Sites To Help You To Become An Expert In Car Key Programer auto key Programmer
What’s The Job Market For Automotive Locksmith Key Programming
Professionals? automotive locksmith key programming (Craig)
10 Facts About Car Key Programmer That Can Instantly Put You In An Upbeat Mood car keys programmed near me
The Worst Advice We’ve Ever Received On Car Key Programmer Car Key Cutting And Programming Near Me (Ns1.Javset.Net)
Hb88 noi len la nha cai uy tin so 1 tai Viet Nam vao dau 6/2019. Nha cai noi tieng voi cac san pham Ca cuoc the thao, game slot.
Website: https://phongee.vn/
Hb88 noi len la nha cai uy tin so 1 tai Viet Nam vao dau 6/2019. Nha cai noi tieng voi cac san pham Ca cuoc the thao, game slot.
Website: https://phongee.vn/
I came across your site wanting to learn more and you did not disappoint. Keep up the terrific work, and just so you know, I have bookmarked your page to stay in the loop of your future posts. Here is mine at QH8 about Cosmetic Treatment. Have a wonderful day!
What’s The Job Market For Automotive Locksmith Key Programming Professionals
Like? program
Why Incorporating A Word Or Phrase Into Your Life Will
Make All The Different programmer
10 Things We All Love About Key Programmers key programmers near me (historydb.Date)
Why Programming Keys Is A Must At The Very Least Once In Your Lifetime fob Key Programming
celebrex 0.025%
It’s The Complete Guide To Program Keys For Cars programming Car key
10 Things That Everyone Doesn’t Get Right About The Word “Car Key Programmer Near Me.” auto car key programmer near me
15 Hot Trends Coming Soon About Automotive Locksmith Key Programming car key programming And cutting
How To Make An Amazing Instagram Video About Programing Keys transponder key Programmer
10 Strategies To Build Your Car Key Programmer Near Me Empire Car Key Programming Cost
9 . What Your Parents Taught You About Key Programmer program
What Is Car Key Programing And How To Utilize What Is Car
Key Programing And How To Use Car Keys Cut And Programmed Near Me
Car Key Programer Explained In Fewer Than 140 Characters Car key programmers
The Ultimate Guide To Reprogramming Car Key key reprogramming
10 No-Fuss Methods To Figuring Out The Key Programmers In Your
Body. car key programmers Near Me
Guide To Car Key Program Near Me: The Intermediate Guide In Car Key Program Near Me Car Key Program Near Me
See What Car Key Programmer Near Me Tricks The Celebs Are Utilizing car key programmer near
me – http://www.daoban.org,
vasotec
The Best Way To Explain Key Programmer To Your Boss fob Key Programmer
10 Car Key Reprogramming Tricks All Experts Recommend reprogramming keys for cars
Key Programming: What’s No One Is Talking About mobile Key programming
15 Of The Best Pinterest Boards Of All Time About Cabin Beds With Storage Cabin bed low
What’s The Job Market For Replacement Lexus Key Professionals?
Lexus key
What’s The Current Job Market For Togel Hongkong Professionals Like?
togel Hongkong
What’s The Current Job Market For Daftar Situs Togel Professionals?
Daftar Situs Togel
10 Upvc Door Hinge Replacement Tricks Experts Recommend window hinge fix
5 Adult ADHD Medication Uk Projects For Any Budget Coping With Adhd Without Medication
10 Healthy Habits To Use Replacement Mazda Key mazda 3 key programming
10 Things That Your Family Teach You About Volkswagen Key Cutting Service Near Me Volkswagen Key Cutting
Service – Morphomics.Science,
You’ll Never Be Able To Figure Out This Car Ignition Switch Repair’s Tricks
car ignition switch repair
20 Reasons Why Replacement Car Keys Peugeot Will Never Be Forgotten Peugeot Partner Key Fob
I am genuinely thankful to the owner of this website for sharing his brilliant ideas. I can see how much you’ve helped everybody who comes across your page. By the way, here is my webpage 92N about Cosmetic Treatment.
The 10 Most Terrifying Things About Programming Car Key
programming
It’s The Next Big Thing In Key Programming Mobile Key programming near me
What’s The Job Market For Sofas And Sectionals Professionals Like?
sofas and sectionals
7 Little Changes That’ll Make An Enormous Difference To Your Togel Singapore togel4d [Silas]
5 Killer Quora Answers On Programing Keys programing key (Lavonne)
Five Killer Quora Answers To Link Togel Resmi link Togel resmi – 47.108.249.16,
What’s The Current Job Market For Automotive Locksmith Key Programming Professionals?
automotive locksmith key programming
This Is The Ultimate Guide To Best Queen Bunk Beds best low Profile bunk beds, isaevclub.Ru,
10 Inspirational Graphics About Key Programmers Mobile Key programmer
9 Signs That You’re A Reprogramming Car Key Expert Reprogramme Car Key
Many Of The Common Errors People Make When Using Car Key Programming
Near Me car key Programing Near me
The 3 Greatest Moments In L-Shaped Bunk Beds For Small Rooms History l shaped Bunk bed
15 Current Trends To Watch For Program Car Keys Car Keys Programmed Near Me
You’ll Never Guess This Situs Togel Dan Slot Terpercaya’s
Benefits Situs togel dan slot Terpercaya
Watch Out: How Replacement Porsche Key Fob Is Taking Over And What To Do About It car key cutting service
10 Program Keys For Cars-Friendly Habits To Be Healthy reprogramming car keys
Bandar Online Togel Tools To Ease Your Daily Life Bandar Online Togel Trick That Every Person Should Know bandar Togel terpercaya
What’s The Current Job Market For L Shape Couches Professionals Like?
l Shape couches
The Reasons Why Adding A Keys Programmed To Your
Life Will Make All The Change programmers
You Are Responsible For The Key Reprogramming Budget? 12 Best Ways To Spend
Your Money programming a key
9 Things Your Parents Taught You About Togel4d Login Togel4D Login
Car Keys Repairs Tools To Improve Your Daily Lifethe One Car Keys Repairs Technique Every
Person Needs To Be Able To car Keys repair
Who Is Situstoto Slot And Why You Should Take A Look
Togel sydney
Are You Getting The Most Value Of Your Sofas In Sale?
2 Seater Couch For Sale
20 Key Programer Websites Taking The Internet By Storm programming
The 12 Best Land Rover Key Fob Accounts To Follow
On Twitter reprogram
Is Programming A Car Key The Greatest Thing
There Ever Was? auto
Toto Online Terbaik Strategies From The Top In The Business Togel sydney
This Is The One Car Keys Programming Trick Every Person Should Be
Able To key fob programmers near me
The 9 Things Your Parents Teach You About Childrens Bunk Bed
childrens Bunk bed (79bo.Com)
Buzzwords De-Buzzed: 10 Different Ways To Say Reprogramming Car
Key Reprogramme Car Key
Are Situs Togel Dan Slot Terpercaya The Best Thing There Ever Was?
toto online Terbaik
11 Methods To Completely Defeat Your Car Key Programer Car key programmers
5 Clarifications On Key Repair Near Me door
key repair near me (Concetta)
“The Ultimate Cheat Sheet For Key Programming Car cut and program car key
Are You Getting The Most You 1 Kg Of Coffee Beans? coffee Beans uk 1Kg
15 Things You Don’t Know About American French Style Fridge Freezer american style fridge freezer french Door
9 Things Your Parents Teach You About Daftar Akun Togel Resmi daftar akun togel Resmi
Why Toto Online Terbaik Is Fast Becoming The Hottest Trend Of 2024?
Bandar Togel Terpercaya
Bandar Online Togel Tools To Make Your Daily Lifethe One Bandar
Online Togel Trick That Everyone Should Know Bandar Online Togel
10 Ways To Create Your Ford Key Empire Ford keyfob
Seven Explanations On Why Situs Togel Dan Slot Terpercaya Is Important Toto Online Terbaik
You’ll Never Guess This Situs Togel Dan Slot Terpercaya’s Secrets situs togel dan slot terpercaya – Travis,
5 Killer Quora Answers To Toto4d toto4d (Felipa)
The Companies That Are The Least Well-Known To Follow In The Togel Singapore Industry togel4D
5 Killer Quora Answers On Daftar Situs Togel daftar situs togel
5 Situs Toto Tips From The Professionals togel Hongkong
7 Small Changes That Will Make The Biggest Difference In Your Situs Togel
Terpercaya togel resmi indonesia (Alphonso)
Guide To Daftar Akun Togel Resmi: The Intermediate Guide In Daftar Akun Togel Resmi
daftar akun togel resmi (Dedra)
Five Coffee Pods Coffee Machine Projects To Use For Any Budget Best coffee pod machine
10 Myths Your Boss Has Regarding Togel Sydney situs togel online; Stacey,
Guide To Situs Togel Dan Slot Terpercaya: The
Intermediate Guide On Situs Togel Dan Slot Terpercaya Situs Togel Dan Slot Terpercaya
The Most Common Ford Focus Replacement Key Cost Uk Mistake
Every Beginner Makes genuine ford key fob
9 . What Your Parents Teach You About Togel4d Login togel4d login
Pragmatic Casino: 10 Things I’d Like To Have Learned Earlier 프라그마틱 공식홈페이지
10 Things That Your Family Teach You About Collapsible Mobility
Scooter collapsible mobility scooter
Five Killer Quora Answers On Situs Terpercaya Situs terpercaya
Toto Online Terbaik Tips From The Best In The Industry Bandar Toto
5 Killer Quora Answers To Situs Togel Online Situs Togel Online (Planforexams.Com)
Bandar Online Togel Tools To Ease Your Everyday Lifethe Only Bandar Online Togel Trick That Every Person Should Be Able To bandar online togel
The 10 Scariest Things About Bifold Door Seal Repair bifold door seal repair
10 Things Everyone Gets Wrong About The Word “Pragmatic.” 프라그마틱 데모
5 Killer Quora Answers On Mesothelioma Attorneys Mesothelioma attorneys
Ten Retro Fridge Freezers Myths That Aren’t Always True Retro American fridge freezers uk
5 Reasons To Be An Online SEO Consultant In London Buyer And 5 Reasons Why You Shouldn’t london seo expert
The Hidden Secrets Of Chest Freezers top rated small chest freezer
14 Cartoons About Adhd Symptoms For Women To Brighten Your Day adult symptoms of adhd
A Rewind: How People Talked About Seo Backlink Building
Software 20 Years Ago auto backlink software (Jacinto)
GSA SER Tips That Will Change Your Life gsa ser reviews
10 Apps That Can Help You Control Your Local Search SEO local search engine optimisation
What’s The Current Job Market For Marketing Content Writer Professionals Like?
marketing content writer – Ervin,
Why The Biggest “Myths” About SEO Services In London Could Be True search engine optimisation company london [Jamie]
10 No-Fuss Methods For Figuring The SEO Experts London You’re Looking
For Search Engine Optimization In London
Make Money Quick Internet Casinos 몰타 에볼루션
The statute of limitations can be complicated by the fact that asbestos-related diseases like mesothelioma can take a long time to appear.
A knowledgeable attorney can assist victims in determining their deadlines and file within them.
Best Childrens Bunk Beds Tools To Improve Your Daily Lifethe One Best Childrens Bunk Beds Trick That Everybody Should Learn childrens bunk bed (Zoila)
Top SEO Agency 101:”The Complete” Guide For Beginners Uk
11 Ways To Fully Defy Your Spare Mercedes Key mercedes key fob programming (Amie)
7 Things You’d Never Know About Pragmatic
Slot Tips 프라그마틱 홈페이지 (Ara)
Don’t Buy Into These “Trends” Concerning Auto Locksmith Near Me Prices Cheapest auto locksmith near me; Shad,
Ten Things Your Competitors Lean You On Search Engine Optimisation seo optimization london;
Nannie,
10 Things Everybody Hates About Pragmatic Slots 프라그마틱 무료
슬롯버프 (Roxanna)
This Week’s Most Popular Stories Concerning Pragmatic Genuine 프라그마틱 무료체험 메타
20 Interesting Quotes About Sectional Sofas sectional
sofas with recliners – Lakeisha –
You’ll Be Unable To Guess Upvc Window Repair Near Me’s
Secrets upvc Window repair near me; http://Www.stes.tyc.edu.tw,
A Provocative Remark About Upvc Doors Repair sliding doors Upvc
Go88 la cong game doi thuong truc tuyen so 1 Viet Nam hien nay voi hon 2 trieu nguoi choi moi ngay tai trang chu Go88 COM. Voi giao dien dep mat, Go88 cung cap kho game phong phu tu ca cuoc the thao, no hu, xoc dia, tai xiu, bau cua, ban ca, xo so, lo de, den cac game bai dac sac nhu xi dach, ba cay, phom, mau binh, tien len
10 Wrong Answers To Common Pragmatic Korea Questions Do You Know
The Correct Answers? 프라그마틱 무료체험 슬롯버프 –
Lavon,
10 Factors To Know Concerning Coffee Beans Uk You Didn’t Learn At School coffeebeans – Patrice,
7 Things You’ve Always Don’t Know About Pragmatic Return Rate 프라그마틱 무료체험, Andreas,
artigo
https://vavadacasino.com
You’ll Never Guess This GSA SER Seo Backlinks’s
Tricks gsa Ser seo backlinks
Sbobet cung cap dich vu ca cuoc voi tat ca cac mon the thao pho bien nhu ca cuoc bong da, quan vot, bong ro, bong chay, cau long, quyen anh, the thao… Ngoai ra day cung la mot nha cung cap Live Casino va tro choi co bac truc tuyen hang dau the gioi https://sbobet.ooo/
How To Optimize The Payday Loan Benefits 다바오
바다 전망 나오는 호텔 (k12.instructure.com)
30 Inspirational Quotes About Local SEO Experts Local Search business
plan b 10mg
Guide To Search Engine Optimisation Services: The
Intermediate Guide For Search Engine Optimisation Services Search engine Optimisation
Получите промокод для 1win и активируйте бонусы на сайте через промокод 1win
Читайте отзывы о lex casino и активируйте бонусы по ссылке лекс казино слоты
Using Least Expensive Bad Credit Personal Loans 월세 보증금 대출
Sunwin la cong game bai doi thuong truc tuyen hoang gia uy tin so mot Viet Nam hien nay. Ra doi tu 11/11/2011 tai Macau, Sun Win tro nen noi bat voi cac loai game bai doi thuong, Tai Xiu Online, No Hu Online, Ban Ca doi thuong,… website: https://sunwin100.net/
Gamebaidoithuong la nha cai hang dau tai Viet Nam, cung cap nhieu tro choi doi thuong hap dan nhu poker, bau cua va slot. Voi giao dien than thien, khuyen mai hap dan va bao mat thong tin tot, Gamebaidoithuong mang den trai nghiem choi game an toan va thu vi. wed: https://top9gamebaidoithuong.com/
Читайте отзывы о lex casino и активируйте бонусы по ссылке обзор лекс казино
Читайте отзывы о lex casino и активируйте бонусы по ссылке лекс казино бонусы
The Us Bank Bailout Plan Is Filled Dangers 소상공인 대출
7 Effective Tips To Make The Most Out Of Your Best Local SEO
Company building
Sharing is caring the say, and you’ve done a fantastic job in sharing your knowledge on your blog. It would be great if you check out my page, too, at UY6 about Advertise.
Three Greatest Moments In Best Link Building
Software History best seo link building software – Reda –
How To Produce Money Through Online Casinos 에볼루션 기후
How To Save Money On Search Engine Optimization Agency Seo Optimization London; Te.Legra.Ph,
Affordable SEO Company London Tips From The Top In The Business business
Five Killer Quora Answers To SEO Tool Vps Vps
7 Simple Tips For Rocking Your Professional SEO Agency seo marketing agency london (Alfie)
What’s The Job Market For Best Content Marketing
Agency Professionals Like? best content marketing agency
(Vilma)
A Step-By-Step Guide To SEO Software Tools From Beginning To End website search engine ranking Software
Guide To What Is A Content Marketer: The Intermediate Guide Towards What Is
A Content Marketer what is a content marketer (Philipp)
Who’s The Most Renowned Expert On Pragmatic Recommendations?
프라그마틱 무료스핀 (Kendra)
A Productive Rant About Mesothelioma Asbestos Claim mesothelioma lawyers (Bianca)
20 Tools That Will Make You Better At Strollers 3 Wheels 3 wheel umbrella stroller, Isiah,
Why Asbestos Attorney Cancer Lawyer Mesothelioma Settlement
Is Relevant 2023 mesothelioma lawsuits (Bart)
15 Reasons To Not Be Ignoring Pragmatic Kr 무료슬롯 프라그마틱; Cortez,
L Shape Leather Settee Tools To Ease Your Daily Life L Shape Leather Settee Trick Every Person Should Learn l shape leather settee (glamorouslengths.com)
7 Simple Strategies To Totally Rocking Your 3 Wheeler Stroller
best 3 wheel stroller with car seat – Darrin
–
Asbestos Attorney Explained In Fewer Than 140 Characters Mesothelioma Lawsuit
10 Things Everyone Makes Up Concerning Glass Repair Crawley Door Repair
What’s The Job Market For Automatic Electric Folding Portable Lightweight Mobility Scooter Professionals Like?
Automatic electric folding portable lightweight Mobility scooter
14 Businesses Are Doing A Fantastic Job At Window Handle
Repair window handles for upvc
The Best Asbestos Attorney Lawyer Mesothelioma Strategies To Make A Difference In Your Life mesothelioma attorney, Chanel,
9 Lessons Your Parents Taught You About Content Marketing For B2b content marketing for
b2b – Chara,
The 10 Most Scariest Things About Door Fitters Maidstone Rear window replacement maidstone
Integrated French Style Fridge Freezer Tools To Make Your Daily Lifethe One Integrated French Style Fridge Freezer Trick That Every Person Must Know integrated french style fridge freezer
(anipi-Italia.org)
9 Lessons Your Parents Taught You About L Shaped Couch L shaped couch
5 Laws That Anyone Working In Underdesk Treadmill Should Be Aware Of Treadmill for under desk
You’ll Never Guess This Best French Door Fridge Freezer Uk’s Tricks Best french door fridge freezer uk
The Worst Advice We’ve Seen About Free Slot Pragmatic Free Slot
Pragmatic 프라그마틱 불법 (Regina)
Why Sectional L Shaped Couch Is Everywhere This Year l
shaped sectionals leather (Franklin)
The Comprehensive Guide To L Shaped Leather Sofas
l shaped Sectional
Guide To Treadmill At Home: The Intermediate Guide In Treadmill At Home treadmill at home [Cathryn]
10 Things That Your Family Teach You About Compact 3 Wheel Stroller compact 3 wheel stroller (Shirleen)
The Expert Guide To Free Slot Pragmatic 프라그마틱 슬롯 무료
Sectional L Shaped Couch Techniques To Simplify Your Daily Life Sectional L Shaped Couch Trick Every Person Should Be Able To sectional l shaped couch (Cora)
L Shape Leather Settee Tools To Improve Your Daily Lifethe
One L Shape Leather Settee Trick Every Person Should Be Able To l shape leather Settee
What’s The Job Market For Fold In Treadmill Professionals?
fold in treadmill
12 Facts About Triple Stroller That Will Get You Thinking About
The Water Cooler compact stroller (travela.lkumc.org)
See What Sectional L Shaped Sectional Tricks The
Celebs Are Using Sectional l shaped sectional
Where Are You Going To Find Sports Toto Prizes Be One Year From What
Is Happening Now? 토토사이트 꽁머니 (Marcelo)
The Often Unknown Benefits Of Three Wheeler Pushchairs best lightweight 3 wheel stroller – Billy –
10 Things That Your Family Taught You About Compact 3 Wheel Stroller
compact 3 wheel stroller (Marco)
3 Common Reasons Why Your Automotive Locksmith
Isn’t Working (And How To Fix It) mobile automotive locksmiths near me (Princess)
See What Composite Door Replacement Lock Tricks The Celebs Are Utilizing composite door replacement lock
Guide To Private ADHD Assessment Online: The Intermediate
Guide For Private ADHD Assessment Online private adhd assessment
online (Christian)
How Do You Explain Curved Couch Sofa To A 5-Year-Old sectional couches near me (Danuta)
15 Fun And Wacky Hobbies That’ll Make You More Effective At Asbestos Mesothelioma Lawyers Mesothelioma Lawsuit (2E0Bu9Hpognvjjwqcfdnwi.Com)
Does Technology Make Sports Toto Better Or Worse? 먹튀검증 사이트
Who Is Window Companies Birmingham And Why You Should
Care window glass replacement Birmingham (nerdgaming.science)
You’ll Never Guess This Small Couch L Shape’s Tricks small couch l shape – Michale –
10 Things You’ve Learned In Preschool That’ll Help You With L Shaped Couch
sofa l shape cheap
Five Killer Quora Answers To L Shape Sofa Small L Shape Sofa Small
10 Sites To Help You Become An Expert In Mesothelioma Asbestos Lawyer mesothelioma
lawyer (Hermine)
Some Of The Most Ingenious Things Happening With Non Asbestos
Causes Of Mesothelioma mesothelioma lawyer (Lisa)
In Which Location To Research Cheap Wood Burning Stove
Online small modern wood stove; Leigh,
See What Bio Fuel Fireplace Tricks The Celebs Are Making Use Of Bio
fuel fireplace (kendoknife9.werite.net)
Why You Should Be Working With This Sash Window Repair
Sash window Repair near me
What’s The Current Job Market For L Shaped Leather Couch Professionals Like?
l shaped leather couch
10 Misconceptions That Your Boss May Have Regarding Small L Shaped
Settee Small L Shaped Sofa
The 12 Best Cheap Locksmith Near Me Accounts To
Follow On Twitter affordable locksmith near me
Who’s The Top Expert In The World On Asbestos Attorney? mesothelioma lawyers (Irwin)
The 10 Most Scariest Things About L Shaped Leather Couch l shaped leather sofa
11 Ways To Destroy Your Upvc Windows And Doors upvc Windows repairs
Why Private ADHD Diagnosis UK Could Be More Dangerous Than You Thought Private adhd assessment gloucestershire
20 Inspiring Quotes About L Shaped Couch recliner sofa
l shape (Fran)
What Is Glass Hinge And How To Use It replacement
hinges for Upvc windows (Pepperstop46.bravejournal.Net)
Indisputable Proof You Need L Shaped Couch Sectional l shaped sofa bed couch
15 Top Pragmatic Casino Bloggers You Should Follow 프라그마틱 불법, Aurelia,
Ten Asbestos Attorneys That Really Improve Your Life asbestos attorneys (Gudrun)
The Little-Known Benefits Of Asbestos Attorney Lawyer Mesothelioma mesothelioma attorneys (Vanessa)
How To Beat Your Boss On Sports Toto Near
Me Today 먹튀검증 커뮤니티 (wx.gityx.com)
How To Tell If You’re Prepared To Asbestos Attorneys Georgia mesothelioma Lawsuit (glbian.com)
10 Steps To Begin The Business Of Your Dream Couches For
Sale Near Me Business modern couch (janec815wzw0.wonderkingwiki.com)
What NOT To Do During The Door Handle Replacement Industry door handle replacements (Mari)
12 Facts About Pragmatic Slots Experience To Make You Think About The Other
People 프라그마틱 정품확인방법
Ten Startups That Will Revolutionize The Sofas L Shape
Industry For The Better Leather sofas l shape – Alena,
This Most Common Ignition Cylinder Replacement Near Me Debate It’s Not As
Black And White As You Might Think ignition lock Cylinder repair
15 Up-And-Coming Pragmatic Free Bloggers You Need To Keep An Eye On 프라그마틱 무료스핀 [Niki]
The Top Reasons Why People Succeed With The Peugeot Key Replacement Near Me Industry
How to get a new peugeot car key
See What Private ADHD Assessment Near Me Tricks The
Celebs Are Using private adhd assessment Near me
7 Things You’ve Always Don’t Know About ADHD Private
Diagnosis Cost Cheap Private Adhd Assessment
Upvc Window Doctor Near Me Tools To Make Your Everyday Lifethe Only
Upvc Window Doctor Near Me Trick Every Person Should
Learn upvc window doctor near me
10 Websites To Help You To Become A Proficient In ADHD Private Assesment private adhd assessment exeter
10 Books To Read On Sectional Couch L Shaped l shaped couch that reclines (Ellis)
What Freud Can Teach Us About Pragmatic Play 프라그마틱 카지노 (Eulalia)
5 Pragmatic Return Rate Lessons From The Professionals 프라그마틱 무료체험
슬롯버프; Danuta,
Think You’re The Perfect Candidate For Doing Upvc Doors Near Me?
Take This Quiz Repairing Upvc Door
20 Fun Infographics About Leather Couches L Shape l shaped couch With recliners (sofa75293.ssnblog.com)
The Biggest Problem With Pragmatic Free Trial Slot Buff, And
What You Can Do To Fix It 라이브 카지노
(Franchesca)
There Are A Few Reasons That People Can Succeed In The Asbestosis Asbestos Mesothelioma Attorney Industry Asbestos Lawsuit
15 Top Pinterest Boards Of All Time About Bioethanol Fire bio-ethanol
fires – Jonah
–
14 Cartoons About How To Check The Authenticity Of Pragmatic To
Brighten Your Day 프라그마틱 체험; Freddie,
The Three Greatest Moments In Asbestos Cancer Lawyer Mesothelioma Settlement History Asbestos Lawyers
10 Meetups About Futon Couch You Should Attend Deep Couch sectional
10 Websites To Aid You Learn To Be An Expert In Toto Result 메이저사이트 순위
It’s Enough! 15 Things About Double Glazing Repair Cost We’re Overheard
repair to double glazed Windows
5 Killer Quora Answers To Bunk Beds Kids bunk beds kids (Jessika)
The 10 Most Terrifying Things About L Shaped Leather Settee
L Shaped Leather Settee
5 Killer Quora Answers To L Shape Sofa With Couch l
shape sofa with couch (Francesco)
Nine Things That Your Parent Taught You About Sofas L Shape Sofas L Shape
What Freud Can Teach Us About Car Key Replacement Service mobile
car key replacement near me (Kristin)
9 . What Your Parents Taught You About Sectional Sofa L Shaped sectional sofa l shaped
11 Creative Methods To Write About L Shape Sofa With Couch l shaped sectional
leather – Tammi,
15 Sectional L Shaped Couch Benefits Everyone Must Be
Able To sleeper l shaped sofa
See What Sofa With L Shape Tricks The Celebs Are Using sofa with
l shape (Couches59941.get-blogging.com)
Ten L Shape Leather Sofas That Really Make Your Life Better l shape leather sofas
(Jolie)
Guide To Freestanding Electric Fireplace: The Intermediate Guide On Freestanding Electric Fireplace standing electric Fireplace
10 Things Everyone Hates About L Shaped Sectional l shape sofa with recliner (Trina)
How To Tell If You’re Ready For Peugeot 207 Key Replacement
peugeot expert key fob
Three Reasons Why 3 Reasons Why Your Loveseat Couch Is Broken (And How To
Repair It) Couch with storage And Bed
Huge Sectional Couch Tools To Help You Manage Your Daily Lifethe One Huge Sectional Couch Trick That Every Person Should Be Able To huge sectional couch
(bethu813sly8.wikimidpoint.com)
Guide To In The Wall Fireplace: The Intermediate Guide For In The Wall Fireplace fireplace (Colleen)
Guide To Double Glazing Misting: The Intermediate Guide On Double Glazing Misting Double glazing misting
Nine Things That Your Parent Teach You About Sofa Couch
For Sale sofa couch for sale
A Trip Back In Time The Conversations People Had About Private
ADHD Assessments 20 Years Ago private Adhd assessment
dublin, buketik39.ru,
Is Small L Shaped Couch The Most Effective Thing That Ever Was?
sleeper couch l shape (Nora)
The 10 Most Terrifying Things About L Shaped Couch Small l shaped couch small;
Candra,
What Will Electric Fire Wall Mounted Be Like In 100 Years?
wall mounted electric fire uk (Lynn)
Everything You Need To Know About Huge Sectional Couch Dos And
Don’ts fold out couch, yerliakor.Com,
Can Private ADHD Assessment Be The Next Supreme Ruler Of The World?
Private Assessment For Adhd Northern Ireland
The 10 Scariest Things About Asbestos Attorney In Virginia
Asbestos Attorneys
5 Laws That Anyone Working In Pvc Window Hinges Should Know window Friction hinges
You’ll Never Guess This SEO Services London Uk’s Tricks seo services London uk
[cotkan.ru]
Private Psychiatrist: The Ugly Facts About Private Psychiatrist Private Psychiatric assessment
See What Asbestos Attorneys Tricks The Celebs Are Utilizing Asbestos attorney
The 12 Worst Types 4d Result Sport Toto Tweets You Follow 먹튀검증 사이트
5 Tools That Everyone In The L Shaped Sectional Sofa Industry Should Be Utilizing l shape sofa with bed (Wilda)
Saab Replacement Key Tools To Ease Your Daily Life Saab Replacement Key Trick That Everyone Should Learn saab 9 3 key replacement
A Comprehensive Guide To Small L Shaped Settee. Ultimate Guide To Small L Shaped Settee cheap l shape sofa
7 Effective Tips To Make The The Most Of Your Mobility Scooter For Sale mobility scooter cheap for Sale
Bandar Online Togel Tools To Help You Manage Your Daily Life Bandar Online
Togel Trick That Should Be Used By Everyone Know
bandar Online togel – enrollbookmarks.com –
Guide To Freestanding Electric Fireplace: The Intermediate Guide Towards Freestanding Electric Fireplace Standing Electric fireplace
What Is The Reason? Toto Is Fast Becoming The Trendiest Thing Of 2024?
먹튀검증 – Emseyi.Com –
What Causes Mesothelioma Other Than Asbestos: A Simple Definition Mesothelioma Attorney
Buzzwords De-Buzzed: 10 Other Ways For Saying Local
SEO Company London link building agency london (Kristopher)
5 Killer Quora Answers On Bifold Door Glass Replacement Cost bifold door glass replacement cost
Ten Things Everybody Is Uncertain Concerning Asbestos Attorney Lawyer Mesothelioma Mesothelioma lawyers
8 Tips To Increase Your Bandar Online Togel Game bandar togel terpercaya
Your Family Will Thank You For Getting This Key
Repair broken car key Repair
5 Real Sexdoll Lessons From The Pros real sexdolls
Ищете vavada слоты? Мы знаем, где найти актуальные игры.
See What Car Keys Programming Tricks The Celebs Are Making Use Of
Programming
Why The ADHD Private Diagnosis Glasgow Is Beneficial For COVID-19 private adhd assessment edinburgh cost
10 Tips For Getting The Most Value From Asbestos Mesothelioma Compensation mesothelioma lawyers
Why We Our Love For 3 Wheel Pushchair Travel System (And You Should, Too!) 3 Wheel pushchairs
Responsible For A Peritoneal Mesothelioma Asbestos Budget?
Twelve Top Ways To Spend Your Money mesothelioma lawyer
Seven Explanations On Why Locksmith For Car Is Important local locksmiths For Cars
How To Beat Your Boss On Asbestos Mesothelioma Asbestos Lawsuits
7 Small Changes That Will Make An Enormous Difference To Your
Best SEO Agency Uk seo ranker agency
Хотите найти актуальное зеркало? Проверьте вавада зеркало для быстрого доступа к игре.
15 Asbestos Attorney Lawyer Mesothelioma Benefits Everyone
Should Be Able To Mesothelioma Attorneys
A Brief History Of Citroen C4 Key Fob Replacement History Of Citroen C4
Key Fob Replacement Citroen keys
Ten Startups That Will Revolutionize The Car Key Programming Near Me Industry For The Better cost Of Programming a car key
17 Reasons To Not Not Ignore Key Programmers key programmers Near
me (Timeoftheworld.Date)
Guide To Chiminea For Sale: The Intermediate Guide The Steps To Chiminea For Sale chiminea for sale
[Rachele]
10 Misconceptions That Your Boss May Have About Key Programming
Car Key Programmer Near Me
10 Things You Learned From Kindergarden Which Will Aid You In Obtaining SEO Marketing Agency London seo company North london
5. Private Psychiatrists In London Projects
For Any Budget private Practice psychology – stonetop3.werite.net –
15 Best Realistic Sex Dolls Uk Bloggers You Need
To Follow best realistic Sex doll
11 “Faux Pas” You’re Actually Able To Do With Your Asbestos Attorney Mesothelioma Asbestos Lawsuits
See What Walkers Rollators Tricks The Celebs Are Making Use Of walkers Rollators
See What Situs Terpercaya Tricks The Celebs Are Using situs Terpercaya
Your Family Will Thank You For Having This Incline Treadmill electric Incline treadmill
10 Great Books On Realistic Sex Dolla Real life sexdoll
Guide To Boot Mobility Scooter In 2023 Guide To Boot Mobility Scooter In 2023 Mobility scooter car boot
See What Asbestos Attorneys Near Me Tricks The Celebs Are Making Use Of Asbestos attorneys
The Worst Advice We’ve Received On Mesothelioma Attorney asbestos lawyer
What Will Replace Nissan Key Fob Be Like In 100 Years?
nissan note key replacement cost uk
20 Inspiring Quotes About Car Key Cut honda pilot key Cutting
5 Laws That Will Help The Asbestos Mesothelioma Lawsuit Industry Mesothelioma Lawyer
10 Websites To Help You To Become A Proficient In Asbestos Attorneys Chicago asbestos Lawsuit
See What Replacement Lock For Composite Door Tricks The Celebs Are Utilizing
replacement lock for composite door (bombertile4.bravejournal.net)
Check Out: How Cheap Realistic Sex Doll Is Taking Over And What To Do About It cheap realistic Sex Dolls
A Provocative Rant About Replacement Upvc Window Handles
replace upvc window handle
Three Of The Biggest Catastrophes In Sports Toto Results The Sports Toto Results’s 3
Biggest Disasters In History 토토사이트 [wuyuebanzou.com]
10 Things That Your Family Teach You About Realisticsexdolls Realisticsexdolls
French Door Fridge Ice Dispenser Tools To Improve Your Everyday Lifethe Only French Door Fridge Ice Dispenser Trick That
Every Person Must Be Able To french door fridge ice dispenser (Maynard)
Guide To Upvc Sash: The Intermediate Guide For Upvc Sash Upvc sash
10 Real Reasons People Hate Electric Wheelchair Fold
Up Folding power Wheelchair
Do Not Make This Blunder On Your Wood Burners Woodburner
See What Sex Dolls Most Realistic Tricks The Celebs Are
Using sex dolls most realistic (mcclanahan-murphy.blogbright.net)
This Week’s Top Stories About Key Programming Car program a key
– Carson,
How To Survive Your Boss On Replacement Porsche Key Fob
porsche key Replica
Играй в самые популярные слоты вавада и получай невероятные бонусы.
The Reasons Why Situs Toto Is The Most-Wanted Item In 2024 togel sydney
Why Ultra Realistic Sex Doll Is Much More Hazardous Than You
Think ultrarealistic sex doll – Shaunte –
Five 1kg Coffee Beans Price Lessons From
The Professionals 1Kg Of Coffee Beans (Maps.Google.Ml)
Toto Online Terbaik Tips From The Top In The Industry Bandar togel Terpercaya (hangoutshelp.Net)
10 Reasons That People Are Hateful To Treadmill Incline Treadmill Incline what do Treadmill incline numbers mean
Here’s An Interesting Fact About Audi Spare Key Audi
replacement Key cost, Historydb.Date,
Ten Asbestos Attorneys That Really Make Your
Life Better asbestos Attorneys
Enough Already! 15 Things About Cleveland Mesothelioma Attorney We’re Tired Of Hearing asbestos lawyer
Seven Reasons To Explain Why Mesothelioma Asbestos Claim Is So Important
mesothelioma attorney
What Mercedes Key Could Be Your Next Big Obsession replacement mercedes keys (kim-sharp.Hubstack.Net)
The Motive Behind Upvc Door Panels Direct Has Become Everyone’s Obsession In 2024
upvc Panel Cut to size
What’s The Job Market For Realistic Sex Dolll Professionals?
Realistic Sex Dolll
Nine Things That Your Parent Taught You About Sexy Doll Realistic Sexy Doll realistic
13 Things You Should Know About Pragmatic That You Might Not Have Known 프라그마틱 정품 사이트 (Philip)
Where Can You Get The Most Reliable Attorney Lawyer Mesothelioma Information? Asbestos Lawyer
5 Laws Anybody Working In Audi Key Should Know replacement audi key Cost
Be On The Lookout For: How Misted Window Repairs Is Taking
Over And What You Can Do About It misted Window repairs Near me
5 Killer Quora Answers On Auto Folding Mobility Scooters Uk
auto Folding mobility scooters
8 Tips To Up Your Wooden Sash Windows Game how Much do wooden sash windows cost – championsleage.review –
Five Killer Quora Answers On Private ADHD Assessment London private adhd assessment london
Window Hinge Repair Near Me: 11 Thing You’re Forgetting To Do Replace upvc window Hinge
The 10 Most Dismal Toto Result Failures Of All Time Could Have Been Prevented 토지노 사이트
Why No One Cares About Asbestos Attorney Asbestos Attorneys
A Step-By-Step Guide To Asbestos Attorneys From Beginning To End mesothelioma Lawsuit
It’s The One Audi A1 Key Replacement Trick Every Person Should Be Aware Of audi
keyless go (petersson-stout-3.blogbright.net)
Guide To Car Key Replacement Audi: The Intermediate
Guide In Car Key Replacement Audi car key replacement audi
Is Bio-Fireplace The Greatest Thing There Ever Was?
Bio Fireplaces
Glass Repair Bedford: What’s No One Is Discussing door glass replacement bedfordshire
See What Reallife Sexdolls Tricks The Celebs Are
Using Reallife Sexdolls
The 10 Most Scariest Things About U Shaped Sectional With Recliners u shaped sectional with recliners
The Reason Everyone Is Talking About ADHD Diagnosis Private This Moment Private assessment for adhd uk
You’ll Never Be Able To Figure Out This French Style Fridge Freezer
With Water And Ice Dispenser’s Tricks French Style Fridge Freezer With Water And Ice Dispenser
The Best Place To Research Upvc Door Hinges Online upvc doors hinges
An All-Inclusive List Of Local Locksmith Near Me Dos And Don’ts local locksmiths Near Me
Ten Reasons To Hate People Who Can’t Be Disproved Peugeot Boxer Key peugeot replacement key fob – Gabriel,
Why You’re Failing At Contemporary Freestanding Electric Fires freestanding inset electric fires
15 Gifts For The Sports Toto 4d Latest Result Lover In Your Life 토지노 커뮤니티
15 Reasons To Not Ignore Mazda 2 Key Fob mazda keyless entry
The 10 Most Terrifying Things About Upvc Repairs Near Me upvc repairs near me
13 Things About Audi Keys You May Not Have Considered
audi Smart key replacement
The 10 Most Terrifying Things About Double Glazing Repairs Near Me
Double glazing repairs Near me
See What Auto Fold Mobility Scooter Tricks
The Celebs Are Utilizing Auto Fold Mobility Scooter
Ten Things You Shouldn’t Post On Twitter Butt Shaped Sex Toy
A Complete Guide To Freestanding Electric Stoves Dos And Don’ts floor standing electric fireplace (okerclub.ru)
Five Killer Quora Answers On Volkswagon Keys
volkswagon Keys
12 Facts About Bentley Continental Gt Key Fob To Make You Think Twice About The Water Cooler replace
10 Things That Your Family Taught You About Smallest Treadmill With Incline treadmill with Incline (chongyoushe.com)
See What Car Key Reprogramming Tricks The Celebs Are Using Key Reprogramming
Undisputed Proof You Need Commercial Espresso Machine espresso coffee machine with milk frother
Best Kids’ Bunk Beds: The Good, The Bad, And The Ugly bunk beds for kids
10 Factors To Know Regarding Depressive Anxiety Disorder You Didn’t Learn In The Classroom anxiety Disorders examples
10 Things You Learned In Kindergarden To Help
You Get Started With Double Glazing Seal Repairs replacing seals On upvc doors, chessdatabase.science,
From Around The Web Here Are 20 Amazing Infographics About Double Glazing Doctors handles
Five Killer Quora Answers To Programing Keys programing keys (Delia)
10 Things That Your Family Taught You About Walking Pad Desk walking pad Desk
Ethanol For Fire Tips That Will Transform Your Life Bioethanol Corner Fireplace;
Olderworkers.Com.Au,
9 Things Your Parents Teach You About Treadmills For Sale UK Treadmills for sale uk
(total-bookmark.com)
See What Composite Door Handle Replacement Tricks The Celebs Are Using Composite door handle Replacement
See What 3 Wheel Stroller Travel System Tricks The Celebs Are Making Use Of 3 wheel stroller Travel system
9 Signs You’re An Expert Treadmill Home Expert Best Treadmills
Ten Things You’ve Learned In Kindergarden That Will Aid You
In Obtaining Sports Toto Past Results 먹튀검증 커뮤니티
10 Ways To Create Your Fiat 500 Key Replacement Cost
Empire Fiat car keys cut
You’ll Be Unable To Guess Small Treadmill With Incline’s Tricks small Treadmill with incline (images.google.is)
The 9 Things Your Parents Teach You About Daftar Akun Togel Resmi daftar akun togel resmi
10 Tell-Tale Signs You Must See To Get A New Audi Key Programming audi keys replacement cost
10 Things That Your Family Teach You About Cheap Couches For Sale cheap couches for sale
The Expert Guide To Timber Sash Windows double glazed timber sash windows
10 Things Everyone Hates About Grey Sectional Sofa Gray Sectional Sofa
15 Shocking Facts About Window Hinge Repairs That You Never Known replace hinges on upvc window
Five Killer Quora Answers On 3 Wheel Stroller Cheap 3 wheel
stroller cheap – Johnny,
See What Treadmill Home Gym Tricks The Celebs Are Using treadmill home (Christy)
Tread Mills Tools To Streamline Your Everyday Lifethe Only Tread Mills
Trick That Everyone Should Learn tread mills – Bridgette –
An Guide To Vehicle Unlock Service In 2023 Car unlocking Service, Willysforsale.Com,
A Look At The Ugly Reality About Tree House Twin Bunk Bed Play area bunk Beds
The Private Diagnosis Of ADHD Case Study You’ll Never Forget private adhd
assessment leeds (Lowell)
It’s Time To Forget Double Glazing Windows Repairs:
10 Reasons Why You Don’t Have It Double glazed windows repairs
How Much Do Best Womans Sex Toy Experts Earn? sex toy
for women (Patricia)
The 10 Scariest Things About Private Psychiatrist Cardiff private psychiatrist uk cost
10 Facts About Symptoms Of Mania And Depression That Will Instantly Put You In A Good Mood identifying signs Of depression
You’ll Never Guess This Misted Double Glazing Repairs
Near Me’s Secrets Double Glazing Repairs Near Me
The 12 Worst Types Progressive Depression Treatment The Twitter Accounts That You Follow depression treatment in pregnancy
The 10 Most Scariest Things About Upvc Door Repairs Near Me
upvc door repairs near me
Misty Window: What’s The Only Thing Nobody Is Discussing fixing
Misted double glazing (telegra.ph)
Five Qualities That People Search For In Every Spare
Audi Key replacement audi a3 key
12 Companies That Are Leading The Way In Toto Asia 토토사이트
Its History Of Sports Toto Past Results 먹튀검증 사이트
What Is The Heck What Exactly Is Double Glazing Repair
Kit? repair double glazed window (http://www.annunciogratis.net)
Are You Responsible For An Fiat 500 Replacement Key Fob Budget?
10 Very Bad Ways To Invest Your Money fiat 500 key not working
15 Terms That Everyone Who Works In Ghost 2 Immobiliser Installation Industry Should Know audi rs3 ghost installer (Brigette)
5 Clarifications On American French Style Fridge Freezer french door Fridge small
Are You Responsible For A Bean To Cup Machine Budget?
10 Fascinating Ways To Spend Your Money bean to cup coffee machine Offers
Why Is There All This Fuss About Sports Toto Check Winning?
메이저사이트 추천
What’s The Job Market For Best Double Bunk Beds Professionals
Like? Best Double Bunk Beds
10 Signs To Watch For To Know Before You Buy Pragmatic
Product Authentication 프라그마틱 추천
What’s The Current Job Market For Double Glazed Window Repairs Professionals?
double Glazed window repairs
The 10 Most Terrifying Things About Rolls Royce Ghost Key Fob Rolls Royce Ghost Key Fob
A Productive Rant About Car Key Programmer locksmith near me
program key fob (Onlines.pro)
20 Trailblazers Are Leading The Way In Audi G28 Audi Remote Key
Bandar Online Togel Tools To Make Your Daily Life Bandar Online Togel Trick Every Individual Should Know bandar online Togel
Don’t Be Enticed By These “Trends” About Wood Burners woodburner near me
(Denisha)
5 Cliches About 4d Sport Toto You Should Avoid 안전놀이터
9 . What Your Parents Taught You About Treadmills For Sale UK
Treadmills For Sale Uk
10 Unexpected Private Psychiatrist Nottingham Tips private Psychologist
See What ADHD Treatment In Adults Tricks The Celebs Are Using Adhd Treatment In Adults
5 Titration ADHD Meds Leçons From The Professionals titration for
adhd – George –
What Freud Can Teach Us About Pragmatic Slots Free Trial 프라그마틱 슬롯 무료체험 (Networkbookmarks.Com)
5 People You Oughta Know In The Depression Treatment Centers Industry depression treatment
in uk; Joel,
Your Family Will Thank You For Having This Kids
Bunkbed bunk beds uk (gdchuanxin.Com)
Are You Getting The Most From Your Daftar Situs Togel?
Situs Togel Online
Five Laws That Will Aid Industry Leaders In Private Psychiatrist Chester Industry private psychological assessment
(Shelia)
The Best Treatment For ADHD Adults Tricks To Change Your Life best treatment for adhd
No Excuses, You Here Is A Professional Poker Set To Play Poker 에볼루션 바카라 잘하는법
14 Smart Ways To Spend Your The Remaining Double Pushchair 3
Wheeler Budget 3 wheeler Pushchair
Add ADHD Medications: Myths And Facts Behind Add ADHD
Medications can i Get adhd medication without a diagnosis
Local SEO Near Me Techniques To Simplify Your Everyday Lifethe Only Local
SEO Near Me Trick That Should Be Used By Everyone Learn local seo near Me
“The Toto Asia Awards: The Best, Worst, And Most Bizarre Things We’ve Seen 먹튀검증 사이트, Parthenia,
Ten Things Everyone Misunderstands About The Word “How Much Does It Cost To Replace A Porsche Key.” porsche
cayenne Replacement key uk – telegra.ph –
12 Facts About Toto Result That Will Refresh Your Eyes At The Water Cooler 안전놀이터 추천
toto togel
Coloringville: Υour Premier Destination fοr Trusted Togel Gaming
Trust Coloringville fоr aⅼl your link togel needs.Ꮤe provide a secure platform for playing togel resmi terpercaya,
enuring ɑ great gaming experience ᴡith evеry visit.
Why Treatments For ADD Doesn’t Matter To Anyone Treatment adhd
5 Pragmatic Free Trial Lessons Learned From Professionals 프라그마틱 체험
Real Life Sexdolls Tools To Help You Manage
Your Everyday Lifethe Only Real Life Sexdolls Trick That Should Be Used By Everyone Know Real Life Sexdolls
10 Facts About Vauxhall Zafira Key Fob Replacement That Will Instantly Bring You
To A Happy Mood how much is a vauxhall Replacement key
What You Should Be Focusing On Making Improvements To Car Seat Buggy 2 In 1 cheap 2 in 1 prams
What’s The Current Job Market For Sleeper Sofas For Sale Professionals Like?
sleeper Sofas for sale (Vikingwebtest.berry.edu)
One Key Trick Everybody Should Know The One Incline Treadmill
Trick Every Person Should Be Able To electric incline Treadmill
5 Qualities People Are Looking For In Every Adhd Assessments get An adhd Assessment
Fold Treadmill Techniques To Simplify Your Daily Lifethe One Fold Treadmill Trick That Everyone Should Be Able To fold
treadmill (Ngan)
You’ll Be Unable To Guess Best Value Bean To Cup Coffee Machine’s Benefits best value bean to cup coffee machine
Guide To Mobile Ignition Lock Repair Services:
The Intermediate Guide In Mobile Ignition Lock
Repair Services Mobile Ignition Lock Repair Services
The 10 Most Scariest Things About Sports Toto Website 토토 꽁머니
An Adventure Back In Time A Conversation With People About Ghost 2 Immobiliser Fitting Near Me
20 Years Ago autowatch ghost installers birmingham
The Little-Known Benefits Of Car Key Replacement Ferrari
Ferrari Replacement Key Cost Uk
Cat Flap Cover For Winter Cat flap cover for Winter
The 10 Most Scariest Things About Folding Treadmill Incline treadmill incline
A The Complete Guide To Pragmatic Return Rate From Start To Finish 프라그마틱 정품 확인법
20 Car Diagnostic Websites That Are Taking The Internet By Storm Diagnostic For Car Near Me
10 Tell-Tale Symptoms You Need To Get A New Programming Car Key Automotive key programmer
The 10 Scariest Things About Treadmill UK Treadmill Uk
Why Replacement Audi Key Isn’t A Topic That People
Are Interested In Replacement Audi Key new audi key
The Main Issue With Upvc Replacement Door Handles, And How To
Fix It door hinges upvc
Where Do You Think Skoda Key Programming 1 Year From In The Near Future?
Skoda Locked Keys In Car (http://Www.Stes.Tyc.Edu.Tw)
Are You Responsible For The Realistick Sex
Doll Budget? 12 Ways To Spend Your Money ultra Realistic silicone sex Doll
Five People You Must Know In The Under Desk Treadmill Industry health And Fitness
10 Tell-Tale Warning Signs You Should Know To Find A
New Audi Keys Audi connect Key
Is Your Company Responsible For A Window Seal Repair Budget?
Twelve Top Ways To Spend Your Money Window seal repair near me (dokuwiki.stream)
Treadmills Sale Tools To Ease Your Daily Lifethe One Treadmills Sale Trick That Everybody Should Know
treadmills Sale
The 10 Most Terrifying Things About Pushchairs 2 In 1 Pushchairs 2 In 1
4d Sport Toto Isn’t As Difficult As You Think 토지노 커뮤니티
Откройте для себя лучшие игры на сайт вавада и выигрывайте каждый день!
Are You Responsible For An Peugeot Key Fob Budget? 10 Ways To Waste Your Money Replacement key for peugeot 308
20 Fun Details About Kia Sportage Replacement Key Kia dealership key replacement,
witchalibi61.bravejournal.net,
10 Quick Tips About Treatments For Adult ADD treating adhd without medication
Unexpected Business Strategies That Aided Adult Toys For Men Succeed male toys (annunciogratis.net)
You’ll Be Unable To Guess Plush Sectional Sofas’s Tricks plush sectional sofas (Gina)
5 Laws That’ll Help Industry Leaders In Replacement Toyota Car
Key Industry toyota aygo replacement key cost uk
The Top Reasons People Succeed With The Electric Fire Wall Mounted Industry White Wall Mounted Electric Fireplace [Able2Know.Org]
10 Best Facebook Pages Of All Time About Upvc Door Doctor Upvc doctor
Guide To Electric Foldable Wheelchair: The Intermediate
Guide In Electric Foldable Wheelchair Electric Foldable Wheelchair
7 Essential Tips For Making The Most Of Your Audi
A3 Key Replacement audi tt key replacement
The Little-Known Benefits Of Compact Treadmill Incline Gym
Could Assessment Adhd Adults Be The Key To Dealing With
2023? Adhd assessment for adults london
The 10 Most Scariest Things About Walking Treadmill Under Desk walking treadmill under desk
What To Look For In The ADHD Test In Adults Right For You testing for Adult adhd
How Double Glazed Window Repair Impacted My Life The Better window repairs near Me
11 Ways To Completely Sabotage Your Window Replacement Aylesbury Window Fitters Aylesbury
Back Door With Cat Flap Fitted back door with cat flap fitted
How To Save Money On Citroen Ds3 Key Replacement citroen c4 picasso key Replacement
14 Questions You Might Be Insecure To Ask About Pragmatic Slots Free
Trial 프라그마틱 플레이
A Toto Success Story You’ll Never Be Able To 스포츠토토 사이트
Guide To Ultra Lightweight Folding Electric Wheelchair:
The Intermediate Guide On Ultra Lightweight Folding Electric Wheelchair Ultra Lightweight Folding Electric Wheelchair
The Most Effective Advice You’ll Ever Receive About Hyundai Key Replacement Near Me
cheapest
10 Things You’ll Need To Be Aware Of Situs Togel Terpercaya Togel Resmi Indonesia
The Cheap Rabbit Vibrators Awards: The Top, Worst, Or Weirdest Things We’ve Ever Seen Sextoys rabbit
Citroen Key Replacement Tools To Facilitate Your Life Everyday auto
The People Closest To Bandar Toto Tell You Some Big Secrets togel Singapore
8 Tips To Increase Your Pragmatic Ranking Game 프라그마틱 사이트
The Secret Secrets Of Upvc Door And Window Repairs Upvc Door And Window Lock Replacements And Repairs
You’ll Be Unable To Guess Audi A3 Replacement Key’s Secrets Audi a3 replacement key
3 Ways The Toto Korea Prize Can Affect Your Life 첫가입 꽁머니
The Most Significant Issue With Toto, And How You Can Solve It 메이저사이트 추천,
bookmarkfavors.com,
20 Trailblazers Are Leading The Way In Double Glazing Repair Kit repair double glazed windows
Cat Flap Installation Cost cat flap installation cost
(Uta)
How You Can Use A Weekly Pragmatic Project Can Change Your Life 무료슬롯 프라그마틱
You’ll Be Unable To Guess Bifold Door Repairs Near Me’s
Secrets Bifold Door Repairs Near Me; Morphomics.Science,
5 Pragmatic Slot Experience Lessons From Professionals 프라그마틱 슬롯 팁
How Much Is A Spare Car Key Tools To Improve Your Everyday Lifethe Only How Much Is A Spare Car Key Trick Every
Person Should Learn how much is a spare Car Key
5 Killer Quora Answers To Bi Fold Door Repairs Near Me bi Fold door repairs near me
A Look At The Secrets Of Adhd Adult Assessment adhd Assessment For adults uk
A Proficient Rant Concerning Black Fridge Freezer which fridge freezer best buy
– Elke
–
5 Double Dildo Toy Lessons From The Professionals Realistic Double Dildo
The 10 Scariest Things About Sash Window Locks With Key sash Window locks with key
Local Business SEO Services 101: The Ultimate Guide For Beginners local Seo service
What’s The Job Market For 3 Wheeled Buggy Professionals?
3 wheeled buggy – maps.Google.Hr –
15 Tips Your Boss Wished You’d Known About Assessment Mental Health General mental health Assessment (80agpaebffqikmu.рф)
20 Best French Style Fridge Freezer Uk Websites Taking The Internet By
Storm french door refrigerator with largest Freezer
What You Need To Do With This Ford Key Fob Replacement ford Focus remote Key
15 Astonishing Facts About Private ADHD Assessment London Private Adhd Assessment Ireland Adult
Why We Are In Love With Audi Key Replacement (And You Should Too!) spare audi key
You’ll Never Guess This SEO Company Near Me’s Benefits Seo Company Near Me
The 9 Things Your Parents Teach You About Repairing Upvc Windows repairing Upvc windows
How To Save Money On Medication For Autism And ADHD Medication For Adhd And Depression –
Mozillabd.Science –
Wall Mount Electric Fireplace Tips That Can Change
Your Life wood fireplace (Carroll)
How The 10 Worst Sports Toto Online-Related FAILS
Of All Time Could Have Been Prevented 안전놀이터
What Will ADHD Private Assesment Be Like In 100 Years?
private adhd assessment dundee
5 Qualities People Are Looking For In Every Double Glazing
Repairs Milton Keynes bifold doors milton Keynes
Who Is The Best Debt Settlement Service To Secure A Loan Coming From?
학생 대출
The Top Land Rover Discovery 4 Key Fob Replacement The Gurus Are Using 3 Things land rover Discovery 3 Key fob case
The Reasons Window Glass Repair Near Me Is Harder Than You Imagine window Repairs
Do Not Buy Into These “Trends” About Outdoor Wood Burner best woodburner Stoves
20 Resources That Will Make You More Successful At On The Wall Fireplace fireplaces wood – Christopher
–
An Easy-To-Follow Guide To ADHD Symptoms In Adult Women adhd with women, Kaylene,
9 . What Your Parents Taught You About How To Repair A Upvc Door How To Repair A Upvc Door
Is Your Company Responsible For The Audi Key Replacement Budget?
12 Ways To Spend Your Money replacement audi a3 key – clinfowiki.win –
The 10 Scariest Things About Tread Mills Tread Mills
See What Asbestos Attorneys Near Me Tricks The Celebs Are Using
Asbestos Attorney
How To Become A Prosperous Sport Toto Official Website When You’re Not Business-Savvy 토지노 커뮤니티
On Minimizing The Hazards Of Online Poker
헝그리샤크 에볼루션 9.1.6 버그판
The No. 1 Question Everybody Working In Sports Toto Prizes Must Know How To Answer 토토사이트 꽁머니
The Most Common In The Wall Fireplace Debate Isn’t As Black And White As You Think ethonal fire (stayr8.com)
0jun888.com Thanh lap thang 8 nam 2021, thuoc tong bo lien minh OKVIP co tru so chinh tai Luan Don – Vuong Quoc Anh, Jun88 hoat dong hop phap va duoc chung nhan tu Isle of Man va Khu kinh te Cagayan and Freeport, hien tai dang mo rong them chi nhanh tai Viet Nam. website: https://0jun888.com/
Many Of The Common Errors People Make Using Mental Health Assessment
London Checklist For Mental Health Assessment
Five Killer Quora Answers To Affordable Link Building Services affordable link building services; Catharine,
The Advanced Guide To Asbestos Mesothelioma Lawsuit mesothelioma lawsuits (yogaasanas.science)
The Most Powerful Sources Of Inspiration Of Chiminea Outdoor chiminea outdoor fireplace
Five People You Should Know In The Walking
Treadmill Under Desk Industry treadmill for under desk, Betsey,
The Most Hilarious Complaints We’ve Been Hearing About Audi Key Replacement
audi smart key replacement
10 No-Fuss Methods For Figuring The Symptoms Of Adhd In Adults Female You’re Looking For Female Symptoms Of Adhd
10 Top Mobile Apps For Window Repair Near Me window repairs near me
Guide To Tilt And Turn Windows Repair: The Intermediate Guide Towards Tilt
And Turn Windows Repair Tilt and turn windows repair
What Is Wall Electric Fireplace And Why Is Everyone Speakin’ About It?
Wall Fires
Question: How Much Do You Know About Sports Toto History?
메이저사이트
This Week’s Most Remarkable Stories About Audi Car Key Replacement Audi Car
Key Replacement replacement key audi (telegra.ph)
The Little-Known Benefits Of Wall Mounted Fireplace ethonal fire, Amy,
10 Healthy Wall Mounted Fireplace Habits Wallfire
Five Killer Quora Answers On GSA SER List gsa Ser
What Is The Best Place To Research Saab Key Replacement Online fob
Mesothelioma is a lethal form of cancer caused almost exclusively by
exposure to Asbestos case.
A New York mesothelioma lawyer can assist families and
victims in holding companies accountable for concealing this dangerous substance.
Asbestos Attorney Lawyer Mesothelioma Tips To Relax Your
Daily Life Asbestos Attorney Lawyer Mesothelioma Trick That Every Person Should Be Able
To asbestos attorney (ywhhg.Com)
The People Closest To 2 In 1 Travel System Uncover Big Secrets 2 in 1 travel system pram
Five Killer Quora Answers To Bifold Door
Glass Replacement Cost Bifold Door Glass Replacement Cost
10 Misconceptions Your Boss Shares Concerning Case Battle
case battle promo
10 Misconceptions Your Boss Holds Regarding Audi A4 Key Replacement
cars
10 Things You’ll Need To Be Educated About Togel Singapore
Togel Hongkong
Responsible For An Free Pragmatic Budget? 10 Fascinating Ways To Spend Your Money 프라그마틱
The 10 Most Scariest Things About How Much Is A Rolls Royce Key
How much is a rolls royce key
Local SEO Services Near Me Tools To Improve
Your Everyday Lifethe Only Local SEO Services Near Me Trick That Everyone
Should Know Local Seo Services Near Me
20 Great Tweets From All Time About Key For Mini Cooper mini cooper lost key
10 Quick Tips For American Style Fridge Freezers american style Fridge freezer cheap
9 Signs That You’re A Bifold Door Repair Expert Bifold door repair Bracket
5 Laws That Can Help To Improve The Case Opening Battles Industry case battle win (Marion)
13 Things About Mesothelioma Asbestos Lawyers You May Not Have Known Mesothelioma lawsuits
Audi A1 Car Key Tools To Ease Your Daily Life auto
10 Healthy Porsche Key Shell Habits Porsche Remote (Singflock8.Bravejournal.Net)
You’ll Be Unable To Guess Togel Hongkong’s Tricks togel hongkong
(Dianna)
The Most Significant Issue With Keys For Mercedes And What You Can Do To Fix It mercedes key
repair (Natasha)
5 Killer Quora Answers To Bi Fold Repairs bi Fold repairs
20 Myths About Attorneys For Asbestos Exposure: Dispelled Asbestos Attorneys
Five Killer Quora Answers To Under Desk Treadmill With Incline under desk treadmill with
incline; http://www.stes.tyc.edu.tw,
The Three Greatest Moments In Asbestos Cancer Lawyer Mesothelioma Settlement History mesothelioma attorneys (Jann)
Why Nobody Cares About 4d Result Sport Toto 스포츠토토 사이트
Guide To Upv Door Hinges: The Intermediate Guide In Upv Door Hinges Upv door hinges
Don’t Make This Silly Mistake When It Comes To Your Electric Motorized
Treadmill electric Incline Treadmill for sale
What’s The Current Job Market For Pellet Stove Fireplace Insert Professionals?
Pellet Stove Fireplace Insert
3 Reasons 3 Reasons Why Your Double Glazing Window Repair Is Broken (And How To Fix
It) Double glazed window repairs near me
Ten Ways To Build Your Audi A3 Key Replacement Empire
audi tt key Case
The Advanced Guide To Fireplace Bioethanol Fireplaces wooden
5 Toto Online Terbaik Projects For Any Budget bandar Togel Terpercaya
You’ll Never Be Able To Figure Out This Upvc Window Repair’s Tricks
upvc window Repair
What Is Private Psychiatrist Nottingham And How To Use
It psychiatrists
You’ll Never Guess This Doctor Window’s Tricks Doctor window
5 Killer Quora Answers On Bi Fold Repairs bi fold repairs (optionhell9.bravejournal.net)
Keonhacai.forum hay con goi la Keo Nha Cai, la 1 trang web cap nhat va cung cap ty le keo do cac nha cai dua ra de nguoi choi du doan ket qua nhung tran dau bong da. Website: https://keonhacai.forum/
It’s Time To Increase Your Case Battles Options case battle cs (Matthew)
10 Things Everybody Hates About Wall Mounted Electric Fires wall hanging fires
Why Treadmills That Incline Is A Must At A
Minimum, Once In Your Lifetime How To Change The Incline On A Treadmill
10 Meetups About Red Retro Fridge Freezer You Should Attend cheap retro fridge freezer (Lenard)
7 Things About Adult Toy Doll You’ll Kick Yourself For Not Knowing beautiful sexdoll – Charity,
How Window Hinges Propelled To The Top Trend In Social Media fix window hinge
Wall Mounted Electric Fireplace Tips From The Most Effective In The Business Wall Fires
$20,000 To $25,000 Unsecured Loan For Good, Average Or Poor Credit
무직자 대출
A Look At The Future What’s In The Pipeline?
Auto Lock Smiths Industry Look Like In 10 Years? mobile Auto locksmiths
7 Simple Changes That’ll Make An Enormous Difference
To Your Volkswagen Keys Replacement volkswagen beetle key replacement (Matilda)
Guide To Mystery Boxes: The Intermediate Guide On Mystery Boxes mystery boxes (Jesse)
Nine Things That Your Parent Teach You About Foldable Cheap Treadmill foldable cheap treadmill
Guide To Treadmills For Sale Near Me: The Intermediate Guide To Treadmills For
Sale Near Me treadmills for sale near me
5 Killer Quora Answers On Private ADHD Assessment London private adhd Assessment london
The 10 Most Terrifying Things About Mystery Boxes mystery box open Game
A Step-By-Step Guide To Selecting The Right Case Opening Battles csgo battle case (Princess)
15 Reasons Not To Be Ignoring Outdoor Chiminea Cast Aluminum chiminea
14 Smart Ways To Spend Your Leftover Case Opening
Battle Budget best Csgo case Battle Sites
Sectional Couch L Shaped Techniques To Simplify Your Everyday Lifethe Only Sectional
Couch L Shaped Trick That Everyone Should Learn Couch L Shaped
The Most Popular Audi A5 Replacement Key Gurus Are Doing Three Things shop
10 Unexpected Glazing Repairs Near Me Tips Double
Glazing Repairs Near Me (Mcmahon-Larkin-4.Hubstack.Net)
Demisting Double Glazing Tools To Ease Your
Daily Life Demisting Double Glazing Trick Every Individual Should Know demisting Double Glazing
Is Case Battle Just As Important As Everyone Says?
best Csgo case Battle sites
The 10 Scariest Things About Free Standing Electric Fireplace wooden fireplaces, fireplace46666.Digiblogbox.com,
The Expert Guide To Audi Car Key Replacement audi A3 key
The Most Prevalent Issues In Case Battles csgo case battle – Tim,
5 Mystery Box Myths You Should Avoid best one Time Mystery Box
ADHD Test In Adults Tools To Improve Your Daily
Life ADHD Test In Adults Trick That Every
Person Should Be Able To adhd test in Adults
Why Toto Is More Risky Than You Think 메이저사이트 바록가기
The No. One Question That Everyone Working In Case Opening Battle Should Be Able To Answer
Casebattles
The 12 Worst Types Of People You Follow On Twitter links tier
Five Killer Quora Answers To Treadmill Near Me Treadmill Near me
The Most Effective Bandar Online Togel Tips To Transform
Your Life bandar togel terpercaya
Looking For Inspiration? Check Out Automated Backlink Builder Software Backlinks Building Software
What’s The Job Market For Treadmills Electric Treadmills
Professionals? Treadmills Electric Treadmills
A Journey Back In Time What People Talked About Tiered Link Building Strategy 20 Years Ago Tier link Building
15 Twitter Accounts That Are The Best To Find Out More About Case Opening
Battles case battle simulator (Ryder)
Your writing style is cool and I have learned several just right stuff here. I can see how much effort you’ve poured in to come up with such informative posts. If you need more input about Thai-Massage, feel free to check out my website at 71N
From All Over The Web 20 Amazing Infographics About ADHD Diagnosing
Diagnosed With Adhd
Five Killer Quora Answers On Situs Toto Situs Toto
You’ll Never Guess This Mystery Boxes’s Tricks Mystery Boxes
5 Killer Quora Answers To Auto Folding Mobility Scooter With Suspension auto folding mobility scooter with suspension (Rodrigo)
Why Install A Double Glazing Cat Flap? double glazing
cat flap (Nola)
Guide To Titration Meaning ADHD: The Intermediate Guide For Titration Meaning
ADHD titration meaning adhd (Rodrick)
What’s The Job Market For Lamborghini Aventador Svj
Key Professionals Like? lamborghini aventador svj key
You’ll Never Be Able To Figure Out This Composite Door Panel Replacement’s Secrets composite door panel
replacement, wifidb.science,
Guide To Double Glazing Near Me: The Intermediate Guide For Double Glazing
Near Me double glazing near Me
Guide To Double Glazing Windows Repair: The Intermediate
Guide Towards Double Glazing Windows Repair double glazing Windows repair
10 Facts About Used Wood Burning Stoves That Will Instantly Make You Feel Good Mood Cheapest Wood
Burning Stove (Srv29897.Ht-Test.Ru)
Do Not Buy Into These “Trends” About Case Battle battle case csgo
Why People Don’t Care About Asbestos Attorney Mesothelioma mesothelioma lawyer (http://www.1moli.top)
10 Things That Everyone Is Misinformed Concerning
Audi Car Key Audi car keys
Why No One Cares About Mesothelioma Lawyers mesothelioma Law firm
See What Audi A1 Car Key Tricks The Celebs Are Making Use Of audi a1 Car key
Why We Enjoy Mystery Box (And You Should Too!) Best one time mystery box
How Do I Explain How Do I Get A Replacement Key For My Audi To A 5-Year-Old audi a5 key fob
5 Killer Quora Answers On Link Togel Resmi Link togel
This History Behind Chiminea Fire Pit Will Haunt You For The Rest Of Your Life!
large chiminea
9 . What Your Parents Taught You About Adhd Assessments For Adults adhd assessments for
adults (http://www.alonegocio.net.br)
The 10 Most Terrifying Things About Link Togel Link togel
The 9 Things Your Parents Taught You About Smallest Treadmill With
Incline smallest treadmill with Incline
5 Clarifications On Ghost 2 Immobiliser Cost
Porsche 911 Ghost Installer
How To Get More Results Out Of Your Bio Ethanol Fireplace
fireplaces wood
You’ll Never Guess This All Terrain Folding Electric Wheelchair Uk’s Tricks all terrain Folding electric Wheelchair
Nine Things That Your Parent Teach You About Composite Front Door Replacement composite Front door replacement
10 Misconceptions Your Boss Shares Concerning Window Hinge Repair Near Me conservatory Door Hinge replacement
This Week’s Top Stories About Nissan Key Fobs nissan micra key programming
Guide To Folding Treadmills With Incline: The Intermediate Guide For Folding Treadmills With Incline folding treadmills with incline
You Are Responsible For The Asbestos Cancer Attorney Budget?
12 Top Ways To Spend Your Money asbestos attorney
16 Must-Follow Facebook Pages For Audi Tt Key Marketers audi Car key replacement cost
3 Common Causes For Why Your Asbestos Exposure Attorney Isn’t Working (And How To
Fix It) asbestos lawsuit
How Top Asbestos Attorney Propelled To The Top Trend In Social Media Mesothelioma lawyers
3 Ways The Spare Audi Key Will Influence Your Life audi Tt key fob not Working
Guide To Cheap Pellet Stoves: The Intermediate Guide
On Cheap Pellet Stoves cheap pellet stoves (selfless.wiki)
You’ll Never Guess This Situstoto Slot’s Secrets Situstoto Slot
Some Of The Most Common Mistakes People Do With Adult Test For ADHD how to test for adhd In adults
10 Failing Answers To Common Fridge Freezer Black Questions: Do You
Know The Correct Answers? best freestanding fridge freezer
(Irwin)
From The Web Here Are 20 Amazing Infographics About Best Folding Incline Treadmill Training
Buzzwords De-Buzzed: 10 Other Ways For Saying Attorney For Asbestos asbestos Attorneys
How Fireplace Wall Mount Rose To Become The #1 Trend On Social Media Ethonal Fire
Beware Of These “Trends” About Toto Result 스포츠토토 사이트
24 Hours To Improve Audi Car Key Replacement Audi Etron Key
You’ll Be Unable To Guess Lost Ferrari Key’s Secrets Ferrari Key
5 Things That Everyone Doesn’t Know About Bio-Ethanol Fireplace
Fireplaces
123B la trang nha cai uy tin hang dau trong linh vuc giai tri truc tuyen. Chung toi tu hao mang den cho nguoi choi mot san choi an toan. skylock.cc
Program Keys For Cars Tools To Ease Your Everyday Lifethe Only Program Keys For
Cars Trick That Every Person Must Learn program keys For
cars, http://www.Google.com.uy,
How To Choose The Right Search Optimisation Online online
Could Foldable Treadmill Be The Key To 2023’s Resolving?
foldable treadmill uk (Murray)
Guide To Car Key Program Near Me: The Intermediate Guide On Car Key Program Near Me Car Key Program Near Me
11 Creative Ways To Write About Case Opening Battles case Battle Csgo
See What Bifold Door Glass Replacement Cost Tricks The Celebs Are Using
bifold door glass replacement cost
5 Killer Quora Answers To Audi A4 Key Replacement Audi A4 Key Replacement
The 12 Most Unpleasant Types Of Cabin Bed With Slide Accounts You Follow
On Twitter Cabin Beds sale
14 Creative Ways To Spend Extra Situs Togel Terpercaya Budget togel resmi indonesia
It’s The Complete Cheat Sheet For Non Asbestos Causes Of Mesothelioma Mesothelioma Lawyer
15 Great Documentaries About Replacement Audi Car Key Audi Key Replacement Cost
20 Resources That Will Make You Better At Electric Fireplace Suites Cheap Electric Fireplace With Mantel – Xintangtc.Com –
20 Myths About Wood Burner Fireplace: Busted Electric Firesuite
10 Things That Your Family Teach You About Leather Couch With Chaise
Leather couch With chaise
The 10 Most Dismal Nissan Qashqai Replacement Key Failures Of All Time Could Have Been Prevented
nissan navara key replacement; proect.org,
You’ll Be Unable To Guess Window Doctor Near Me’s Tricks
window Doctor near me
Mazda 3 Key Fob’s History History Of Mazda 3 Key Fob
lost mazda Keys
14 Cartoons On SEO Agency Near Me To Brighten Your Day seo agency leicester (Danae)
13 Things About Tier Link Building You May Not Have Known tiered link building
The Little Known Benefits Of Diagnosis ADHD adhd private diagnosis near me
Bandar Togel Terpercaya Tools To Improve Your
Daily Life Bandar Togel Terpercaya Trick That Every Person Must Be
Able To bandar Togel Terpercaya
Why Asbestos Mesothelioma Might Be Your Next Big Obsession asbestos lawyer (korea222.com)
This Week’s Top Stories Concerning Sports Toto Statistics 안전놀이터 순위
Cat Flap Double Glazing cat flap in upvc door cost (Gregory)
Repair Hole In Composite Door Tools To Improve Your Daily Lifethe One Repair Hole In Composite Door Trick Every Individual
Should Learn Repair Hole In Composite Door
Why Nobody Cares About Search Engine Optimisation Agency search engine optimization pricing
15 Things To Give That Pragmatic Kr Lover In Your Life 프라그마틱 슬롯 추천
5 Killer Quora Answers On Window Handle Repair
upvc Wooden window handles
The 10 Most Terrifying Things About Rolls Royce
Phantom Key Fob Rolls Royce Phantom Key Fob
Guide To Replacement Key For Audi: The Intermediate Guide The Steps To Replacement Key For Audi key For audi
Five Killer Quora Answers To Audi A4 Key Replacement audi a4 key
Replacement (Bbs.pku.edu.cn)
Ghost Immobiliser Problems Tips From The Best In The Business bmw x6 ghost Installer
How Much Do Glazing Repairs Near Me Experts Make? double glazing repairs (Bysee3.com)
Five Killer Quora Answers On Walking Machine Under Desk
walking machine under desk
Looking Into The Future What’s In The Pipeline? Private Psychiatrist Glasgow Industry Look Like In 10 Years?
cost of private psychiatrist uk; shakeshare4.Bravejournal.net,
Why All The Fuss About Adhd In Adults Symptoms? ocd and adhd symptoms
Beware Of These “Trends” About Fiat Key Fiat multipla Key
10 Healthy Habits For Bentley Key Replacement
Bentley key fob Repair
The Reasons Audi A1 Key Replacement Is Everyone’s Passion In 2023 audi Key replacement Near Me
Where Can You Find The Most Reliable Espresso Coffee Maker Information? Espresso Coffee Machines
25 Surprising Facts About Case Battles case
battle fun; infozillon.Com,
14 Cartoons About Cheap Wood Burning Stoves That’ll Brighten Your Day
wood Burner for shed
Adding A Cat Flap To Your Bifold Doors cat flaps
10 Life Lessons We Can Take From Window Companies Manchester double glazing installers manchester
20 99 Litre Chest Freezer Websites Taking The Internet By Storm Chest Freezers For Garages Uk
Seo Optimisation Techniques To Simplify Your Daily Life Seo Optimisation Trick
That Every Person Should Know Seo optimisation
Ten Easy Steps To Launch Your Own Saab 9-3 Replacement Key Business saab key Battery Replacement
The Top Companies Not To Be Monitor In The Folding Treadmill With
Incline Industry how to change the incline on a treadmill; Latashia,
A Step-By Step Guide To Private Adult ADHD Diagnosis private adhd assessment warwickshire
You’ll Never Be Able To Figure Out This Free Standing Electric Fireplaces’s Tricks fire
The 10 Most Terrifying Things About Upvc Doors Hinges
upvc doors hinges (botdb.win)
Need Inspiration? Check Out Mobile Diagnostic how much Is car diagnostic test
Treadmill Near Me Tools To Help You Manage Your Daily Life Treadmill Near Me Trick That Everybody Should Learn treadmill near
Me (totalbookmarking.com)
10 Mobile Apps That Are The Best For Electric Freestanding Fire Suite Electric Fireplaces With Mantel (Zenwriting.Net)
The 3 Greatest Moments In Slim Wine Refrigerator History top rated wine fridge (bookmarkhard.com)
15 Things You’re Not Sure Of About Americanfridge Freezer american fridge freezer built in
Why We Do We Love Bedford Double Glazing (And You
Should, Too!) double glazing bedford; Harry,
15 Funny People Working Secretly In Wood Burner hottest wood stove
Five Killer Quora Answers On All-Terrain Stroller Lightweight All-terrain stroller Lightweight
15 Best Pinterest Boards Of All Time About Door Fitter Luton glass window repair
What’s The Current Job Market For American Fridge Freezers Professionals?
Fridge Freezer
20 Important Questions To Have To Ask About Audi Keys Before Purchasing It services
7 Things About Audi A4 Key Replacement You’ll Kick Yourself For Not Knowing replace audi key fob
Five Killer Quora Answers On Upvc Door Lock
Repair Near Me Upvc Door lock repair Near me
10 Pragmatic Slot Manipulation Projects Related To Pragmatic Slot Manipulation To Extend Your Creativity 프라그마틱 무료체험
How To Beat Your Boss On Repair Double Glazing double Glazing repairs
Built In Fridge Freezer The Process Isn’t As Hard As You Think Integrated Fridge Freezer Sale
20 Up And Coming Remote Control Anal Butt Plugs Stars To Watch The Remote
Control Anal Butt Plugs Industry olug anal
The 10 Most Scariest Things About Cheap Sofas For Sale cheap sofas for Sale
What’s The Ugly Truth About Fold Away Treadmill treadmills that
fold up (webwiki.co.uk)
The Best Private ADHD Assessment Edinburgh Strategies
For Changing Your Life private adhd Assessment York
11 “Faux Pas” Which Are Actually Okay To Make With Your Wall Mount Fireplaces Modern Fireplace (Bookmarkspecial.Com)
You’ll Be Unable To Guess Ai Sentence Rewriter’s Tricks ai sentence rewriter
20 Trailblazers Are Leading The Way In Sports Toto Online 먹튀검증 사이트
The 3 Greatest Moments In Mercedes Spare Key History Mercedes Keys
Unexpected Business Strategies Helped Mesothelioma Asbestos Claim
Succeed mesothelioma lawsuit
This Is The Advanced Guide To Pellet Stoves Used Pellet Stoves For Sale
What’s The Point Of Nobody Caring About Upvc Doors Leeds upvc door repair Meanwood
5 Killer Quora Answers On Composite Door Glass Replacement
composite Door Glass Replacement – galloway-boye.technetbloggers.de
–
Guide To 3 Wheel Pushchair Travel System: The Intermediate Guide
The Steps To 3 Wheel Pushchair Travel System 3 wheel pushchair travel
system (yxhsm.net)
20 Trailblazers Setting The Standard In Compact 3 Wheel Stroller 3 wheel pushchair with car Seat
10 Inspirational Graphics About Mesothelioma Claim Mesothelioma Law
Why We Why We Huge U Shaped Couch (And You Should Also!) large u shaped sofa (notabug.Org)
The 10 Most Terrifying Things About Treadmills For Sale UK treadmill
5 Replacement Upvc Window Handles Projects For Any Budget repairing upvc windows
The 10 Most Terrifying Things About Electric Fireplace Heater Free
Standing freestanding Electric fireplace heater
Five Killer Quora Answers To Bifold Door Repairs Bifold door
repairs – Aboutdirectorofnursingjobs.com –
How To Resolve Issues With Situs Togel Online bandar Toto
5 Myths About Upvc Doors Repair That You Should Stay Clear
Of replacing upvc door locks
The 10 Most Scariest Things About Electric Fire Media Wall Electric Fire Media Wall
17 Signs You Work With Asbestos Mesothelioma Mesothelioma Attorneys
Nissan Juke Key Fob Replacement: The Ugly Truth About Nissan Juke Key Fob Replacement nissan car key (Katrina)
Are You Making The Most You Fireplace On Wall?
tabletop fireplace (Nila)
“Ask Me Anything:10 Responses To Your Questions About Link Togel togel Sydney
Are Treadmills On Sale As Important As Everyone Says? saving
The 10 Scariest Things About Cheap Fridge Freezer 50 50 cheap Fridge freezer 50 50
It’s The Evolution Of Bunk Bed Treehouse Treehouse Bed Uk; Tvsocialnews.Com,
15 Gifts For The Electric Wall Mounted Fire Lover In Your Life Electric fire on The wall
The People Nearest To Fiat Key Fob Replacement Uncover Big Secrets nearest
10 Failing Answers To Common Electric Treadmill Foldable Questions Do You Know Which Ones?
electric treadmill under $200 (Melaine)
Why Double Glazing Windows Bristol Is The Next Big
Obsession double glazing bristol
Why The Adhd Symptoms Is Beneficial In COVID-19? list of adhd symptoms
Don’t Forget Audi Car Keys: 10 Reasons That You
No Longer Need It audi smart key replacement
Mesothelioma attorneys aid victims and their family members throughout the legal process.
They prepare cases, file lawsuits and asbestos settlement trust claims they negotiate settlements and fight for fair verdicts in court.
How To Outsmart Your Boss On Chest Freezer Near Me chest Freezer with Drawers Uk
Welcome to DinoGame.app, your ultimate destination for playing the beloved Dino game even when you’re offline
Guide To Affordable SEO Services Near Me: The Intermediate
Guide On Affordable SEO Services Near Me affordable seo Services near Me
See What Asbestos Attorneys Near Me Tricks The Celebs Are Utilizing asbestos attorneys
Vnxoso là nhà cái uy tín số 1 châu Á với hàng trăm game cá cược trực tuyến hàng đầu. Những sản phẩm chính mà Vn Xoso cung cấp phải kể đến cá cược thể thao, Live Casino, đá gà, bắn cá, xổ số, slot game, game bài.https://vnxoso-web.com/
How To Find The Perfect Fridge Freezers Retro Online Cheap retro fridge freezer Uk
Bandar Online Togel Tools To Improve Your Daily Life Bandar Online Togel Trick
That Everyone Should Know Bandar Online togel
Fast Track Your Journey To Online Success 디지몬 어드벤처 라스트 에볼루션 다시 보기
Run 3 is the perfect game for you, where you guide a character through an ever-changing, obstacle-filled space tunnel. With the upgraded version now available at run3.app, your gameplay experience will be even more exciting with new features and smoother mechanics. wedsite: https://run3.app/
What Freud Can Teach Us About Singles Mattress Mattresses Single
Cardiagtech is your go-to resource for all things automotive diagnostics. We offer top-quality car diagnostic tools, including car scan tools and car code readers, along with comprehensive car repair manuals .
20 Questions You Must Always Ask About Small Business SEO Services Before You Buy Small Business SEO
Services Professional seo services
The Federal Reserve Bank – America’s Biggest Unspoken Problem 공무원 대출
888b tu hao la thuong hieu moi phat trien nhanh nhat trong linh vuc ca cuoc doi thuong trong suot 6 nam qua. Tham gia vao nha cai, ban se duoc tan huong nhung tro choi chat luong cao voi ty le tra thuong minh bach va cong bang.
link vào 8live tai https://8live.cool/, nguoi choi co co hoi nhan khuyen mai nap dau len toi 10.000.000d cung nhieu uu dai khac. 8live cam ket bao mat tuyet doi va thanh toan nhanh chong!
It’s The One Best Local SEO Agency Trick Every Person Should Know On Page
10 Healthy Habits For Best Local SEO Agency nearby
15 Twitter Accounts That Are The Best To Learn More About Link Building Agency Uk search engine
optimization Agency – fitch-james.mdwrite.net,
For quick activation, download kmspico activator.
5 Laws Everybody In Organic SEO Agency Should Be Aware Of
Seo marketing agency
Cookie Clicker Unblocked at Cookieclickerunblocked.co is an exciting and addictive game that’s perfect for passing the time. Whether you’re a casual player or someone who enjoys strategy and idle games, Cookie Clicker offers a delightful experience that will keep you hooked for hours. Website: https://cookieclickerunblocked.co/
How May I Lower My Credit Card Interest Fee? Faqs 다바오 충전 방법
Hi there, I simply couldn’t leave your website without saying that I appreciate the information you supply to your visitors. Here’s mine YW9 and I cover the same topic you might want to get some insights about Airport Transfer.
Рекомендуем – популярные бренды курток мужских
Рекомендуем – топ мужских пуховиков
Рекомендуем – лучшие пуховики для мужчин бренды
Private Party 부산달리기 – firsturl.de,
The 9 Things Your Parents Taught You About GSA SER Ranker Gsa ser ranker
VN88 đã xây dựng được lòng tin trong cộng đồng cá cược và trở thành một trong những nhà cái uy tín hàng đầu năm 2024.
Website: https://vn88.company/
#vn88, #nhacaivn88, #vn88company
5 Must-Know Hismphash Practices You Need To Know For 2023 Seo Agency manchester
Рекомендуем – идеи костюмов
The 10 Most Scariest Things About SEO Marketing Company London seo marketing
company; Vicky,
Рекомендуем – тематика хэллоуина
Рекомендуем – halloween costume party
This Week’s Most Popular Stories About Local SEO Expert Local Seo Experts
Guide To Cot Bed Wood: The Intermediate Guide For Cot Bed
Wood cot bed wood
You’ll Never Guess This Best Cots For Newborns’s Tricks Best Cots for newborns
Who’s The Top Expert In The World On Best French Door Fridge Freezer
Uk? French Door fridge australia
Say “Yes” To These 5 ADHD Diagnosis Private Tips private Adhd assessment worcestershire
Test: How Much Do You Know About Audi A3 Replacement Key?
Audi Key Replacement Cost
Why You Should Concentrate On Enhancing Pragmatic Game 라이브 카지노; Ludie,
10 Things We Hate About Pvc Window Hinges Upvc door hinge removal (Olderworkers.Com.au)
What’s The Current Job Market For Remote Key Fob Repair Professionals?
remote Key fob repair [dudoser.Com]
16 Must-Follow Instagram Pages For 2 Seater Fabric Sofa Sale-Related Businesses 2 seater fabric Couch
5 Laws Anyone Working In Rubber Threshold Wheelchair Ramp Should Be Aware Of Van ramp for wheelchair (Cameradb.Review)
Are You Responsible For A Accident Attorney Budget?
Twelve Top Ways To Spend Your Money accident and Injury
“The Bean Coffee Machine Awards: The Best, Worst And Most Bizarre Things We’ve Seen Bean To Cup Maschine
You’ll Be Unable To Guess Best All Terrain Pushchair Uk’s Tricks All Terrain Pushchair Uk
Ten Things You Learned In Kindergarden That Will Help You With Free Slot Pragmatic 프라그마틱
What’s The Reason? Private Psychiatric Assessment Sheffield Is Everywhere This
Year adhd Assessment Psychiatrist
What’s The Job Market For Treadmill Foldable Electric Professionals Like?
treadmill foldable electric
Say “Yes” To These 5 2 Seater Fabric Tips Fabric 2 Seater Sofas (Chanel)
Mesothelioma Legal Question Tips From The Top In The Industry
Mesothelioma attorney
15 Unquestionably Good Reasons To Be Loving UK Private ADHD Diagnosis private adhd Assessment harrogate
Looking Into The Future What’s In The Pipeline?
Pragmatic Industry Look Like In 10 Years? 프라그마틱
Five Killer Quora Answers To Wooden Sleigh Cot Bed wooden sleigh cot Bed
20 Tools That Will Make You More Efficient With
Freestanding Electric Fire Suite free Standing electric fireplace with mantel
15 Incredible Stats About Best Slot Payouts Legitimate slots
Which Website To Research Wall Mounted Fireplace Online on the wall electric fires, maps.Google.com.ua,
Guide To Slot Volatility: The Intermediate
Guide Towards Slot Volatility slot volatility (Danelle)
9 Things Your Parents Teach You About Indoor Chiminea Indoor Chiminea
Do You Think You’re Suited For Link Building Agency Uk?
Check This Quiz Seo agency hertfordshire
Casino Online Crypto It’s Not As Hard As You Think crypto casino online
Beware Of This Common Mistake When It Comes To Your Ghost
Immobiliser 2 audi rs6 ghost installer (Coy)
10 Facts About Toyota Replacement Car Keys That Insists On Putting You
In An Optimistic Mood Toyota estima key fob
15 Gifts For Your Wall Mounted Electric Fires Lover In Your Life
best wall Mount electric fireplace
Audi Replacement Car Keys: The Good, The Bad, And The Ugly audi replacement Keys
7 Secrets About Audi A1 Key That No One Will Tell You Replacement key audi
Guide To Dark Wood Sleigh Cot Bed: The Intermediate Guide The Steps
To Dark Wood Sleigh Cot Bed dark wood sleigh cot bed (Bob)
A Look At The Ugly Facts About Organic SEO Agency local seo Agency
Sage Advice About How To Check The Authenticity Of Pragmatic From
A Five-Year-Old 프라그마틱 이미지
The 10 Most Scariest Things About Best Infant Cribs
best infant Cribs
Upvc Door Panels With Cat Flap upvc door panels with cat flap (Sondra)
Three Reasons To Identify Why Your Item
Upgrader Isn’t Working (And The Best Ways To Fix It) item
upgrades (Bianca)
14 Cartoons On Nissan Juke Key Fob Replacement To Brighten Your Day Nissan micra replacement key (ai-db.science)
Five Killer Quora Answers On L Shape Sofa With Couch l shape Sofa with couch
Fiat Doblo Key Fob Replacement’s History History Of Fiat Doblo Key Fob Replacement
spare
Volvo Keys Explained In Fewer Than 140 Characters
volvo keys explained – Lien –
5 Wooden Cot And Bed Projects For Any Budget wooden cot Bed
Guide To Saab Replacement Keys Uk: The Intermediate Guide The Steps
To Saab Replacement Keys Uk Saab Replacement Keys Uk
15 Reasons You Shouldn’t Be Ignoring Bi Fold Door Repair bifold door repair
What Is The Evolution Of Window Glass Repairs blown
Check Out: How Mystery Box Is Taking Over And How To Stop It Best one Time mystery box
10 Reasons That People Are Hateful Of Cot Bed Sales Cot Beds
The 12 Most Popular Bio-Ethanol Fireplace Accounts To
Follow On Twitter ethanol Fireplaces
What’s The Job Market For Repair Double Glazing Professionals Like?
Repair Double Glazing
10 Great Books On Double Glazed Window Repair window repairs near me
5 Killer Quora Answers To Outdoor Pellet Stove Outdoor Pellet Stove
5 Killer Quora Answers On Bi Folding Door Repair bi folding Door Repair
The Reasons 4 Seater Chesterfield Is More Difficult Than You Think antique chesterfield sofa (Audrea)
Looking For Inspiration? Try Looking Up Ethanol Fireplace Fuel Bio-ethanol Fireplace
Seo Specialists – Tips That Work jusojula
You’ll Never Guess This French Door Refrigerator With Ice
Maker’s Secrets French door refrigerator with ice maker (bookmarkpagerank.com)
Five Killer Quora Answers On Local SEO Service
seo Service
You’ll Never Be Able To Figure Out This Cot Sets’s Tricks cot sets
Guide To Corner Sofa Recliner Fabric: The Intermediate
Guide For Corner Sofa Recliner Fabric corner Sofa recliner fabric
10 Things You Learned In Kindergarden They’ll Help You Understand Sports Toto Online
메이저사이트 추천
Dating Secrets For Men – The Right Way To Pick Up Women Anywhere You Go 오피; ucgp.jujuy.edu.ar,
How Much Do Search Engine Optimization Agency Experts Make?
Seo Agency Leicester
Sports Toto Website: It’s Not As Expensive As You Think
스포츠토토 사이트 (Pr8bookmarks.com)
The 10 Most Scariest Things About Pellet Stoves Near Me pellet stoves near me
What’s The Current Job Market For Pellet Stoves For Rvs Professionals?
pellet stoves for rvs – Bbs.Sanesoft.cn,
Why SEO Marketing London Is A Lot More Risky Than You Thought london Seo
Why Everyone Is Talking About Private ADHD Test Right Now private adhd assessment stoke
on trent (Louvenia)
Learn Zynga Poker Rules Currently – A Breakdown Of The Game
필리핀 다바오 치안
A Help Guide To Private ADHD From Beginning To End private assessment for adhd cost
5 Killer Quora Answers On Toto4d toto4d
9 Things Your Parents Taught You About Renault Clio Spare
Key Renault Clio Spare Key
Guide To Wooden Cot Bed Uk: The Intermediate Guide To Wooden Cot Bed Uk wooden cot bed uk [Everette]
How You Can Use A Weekly Replacement Nissan Key Fob Project Can Change Your Life nissan key repair (Chardindia2.werite.net)
Small 2 Seater Fabric Sofa Tools To Help You Manage Your Daily Life Small 2 Seater Fabric Sofa
Trick Every Person Should Learn small 2 seater Fabric sofa
A Productive Rant About Upvc Window Repairs window repairs Near me
10 Things That Your Family Teach You About Two Seater Fabric Sofa Uk two
seater fabric sofa uk [http://www.Hondacityclub.com]
Cat Flap Installation Near Me cat flap installation near me – Christal,
See What Mitsubishi Remote Key Replacement Tricks The Celebs
Are Using mitsubishi remote key Replacement
A An Instructional Guide To Baby Crib From Beginning
To End great Crib
10 Quick Tips To Mini Cooper Car Key Replacement mini f56 replacement key
Check Out: How Vauxhall Astra Key Is Taking Over The
World And How To Respond vauxhall key fob
7 Useful Tips For Making The Most Of Your Bedford Door Panels
replacement upvc windows Bedford
The 10 Scariest Things About Cot Sales cot sales, Clark,
5 Laws That Anyone Working In Hire Truck Accident Lawyer Should Know truck accident attorney
(Benny)
7 Helpful Tips To Make The Most Out Of Your Sports Toto Korea 스포츠토토
사이트 (Candice)
17 Signs You Work With Key Programming mobile key programming (Swen)
9 . What Your Parents Teach You About Comfortable Couches For Sale comfortable couches for sale (Lesley)
This Is The Frost Free Fridge Freezer 50 50 Case Study You’ll Never Forget Fridge freezer 50
50 sale; frydge-uk50807.Blog-kids.com,
11 Strategies To Completely Block Your Walking Treadmill
Under Desk equipment
Guide To Sex Dolls Lifelike: The Intermediate Guide
For Sex Dolls Lifelike sex dolls lifelike
Five Reasons To Join An Online Chiminea Outdoor And 5 Reasons
You Shouldn’t chiminea outdoor fireplace (Carmine)
What’s The Current Job Market For Ghost Immobiliser Installation Near Me Professionals?
Ghost Immobiliser Installation Near Me
What Is The Future Of Chesterfield Leather Sofa 2 Seater Be Like In 100 Years?
chesterfield leather 2 seater [Elma]
A Step-By’-Step Guide For Citroen Ds3 Key Replacement Citroen Relay Key Fob
17 Signs That You Work With Sectional Sofa Sale Single couches For Sale (euro2020ticket.net)
Why The Asbestos Attorneys Is Beneficial For COVID-19 mesothelioma lawyers (Stephanie)
Toyota Car Key Replacement Tips From The Top In The
Industry new car key toyota
It’s The Evolution Of Bio Fuel Fire biofuel fireplaces
9 Lessons Your Parents Teach You About Cheap Cots cheap cots
You’ll Never Guess This Truck Accident Lawyers’s Secrets semi Truck accident attorney near me
The Best Way To Explain Fireplace Bioethanol To Your Boss fireplaces Shop
What Is Jaguar Key Programming And How To Use It? Jaguar Xf Not Recognising Smart Key
7 Simple Strategies To Completely Rolling With Your Wood Burning Stoves wood burner stove Sale
20 Top Tweets Of All Time About Coffee Machine Best Best espresso machine under 200
See What Accident And Injury Attorneys Tricks The Celebs Are Using accident and injury attorneys
The Best Way To Explain French Door Fridge On Sale To Your Boss french door Fridge with ice maker no Plumbing
20 Things You Need To Know About Audi A4 Key Replacement Audi A4 Replacement Key
Where Do You Think Twin Pushchairs Be One Year From Now?
double Pushchair
Audi Key It’s Not As Hard As You Think replacement Audi a4 Key
10 Facts About Tiered Backlinks Service That Will Instantly Set You In A Positive Mood tier backlink [Dorris]
Online Cryptocurrency Casino Tools To Ease Your Daily
Lifethe One Online Cryptocurrency Casino Technique Every Person Needs To
Be Able To Online cryptocurrency casino
10-Pinterest Accounts You Should Follow About Local SEO London seo professional london (Kaylene)
What’s The Current Job Market For SEO Company In London UK
Professionals? seo company in london uk (Hildred)
You’ll Never Guess This Private ADHD Assessment Near Me’s Secrets Private Adhd Assessment Near Me
5 Killer Quora Answers To Fold Flat Treadmill Fold flat treadmill
9 Lessons Your Parents Teach You About Wood Burning Stove
Modern Wood burning Stove modern
You’ll Never Guess This Truck Accident Compensation’s Tricks Semi truck accident lawyer near me
8 Tips To Improve Your Fiat 500 Key Replacement Cost Game how to get a new fiat 500
key (cameradb.Review)
10 Things That Your Family Teach You About Mini
Cooper Key Fob Replacement replacement mini Cooper key
10 Things You Learned In Kindergarden Which Will Aid You In Obtaining
Wall Mounted Electric Fireplaces white wall mounted electric fireplace
5 Mini Cooper Replacement Keys Lessons From The Pros Mini Smart Key
Treadmill Incline Foldable Tools To Improve Your Everyday Lifethe Only Treadmill Incline Foldable Trick That Every Person Should Learn Treadmill Incline foldable
10 Meetups About Renault Key Card Replacement Near Me You Should Attend Renault Key Card Problems
7 Little Changes That Will Make An Enormous Difference To Your Audi
Replacement Car Keys replacement audi key Cost; yogaasanas.science,
5 Retro Espresso Machine Projects For Any Budget Espresso maker for home
11 Ways To Completely Sabotage Your Lexus
Key Shell repairing
The Best Automatic Folding Mobility Scooters Tricks
To Transform Your Life best automatic folding mobility scooter
Are You Sick Of Unique Slots? 10 Inspirational Sources That Will Revive Your Passion slot Symbols
The 10 Most Terrifying Things About Electric Fireplace Electric fireplace (socialbuzzmaster.Com)
You’ll Never Guess This 3 Wheeled Strollers’s
Tricks 3 Wheeled strollers
5 Killer Quora Answers On Infant Cot Bed infant cot Bed – http://www.northwestu.edu,
Skoda Car Key Explained In Fewer Than 140 Characters skoda car key not working
You’ll Never Guess This Private ADHD Assessment Near Me’s Benefits private adhd assessment near me
Why Is This Mesothelioma Attorney So Beneficial? For COVID-19 mesothelioma Legal
Are You Tired Of Renault Key Replacement? 10 Inspirational Sources That Will Rekindle Your Love renault
Car key replacement cost (telegra.ph)
20 Things You Should Know About Fireplace On Wall electric Fires
Upvc Door Locks Eastleigh Tools To Make Your Daily Life Upvc Door Locks Eastleigh Trick Every Person Should Be Able To Upvc door locks eastleigh
7 Essential Tips For Making The Best Use Of Your Psychiatric
Assessment Form assessment of psychiatric patient (Marcus)
What’s The Reason? Windows And Doors Leeds Is Everywhere This Year Condo window Repair
5 Lessons You Can Learn From Audi A3 Replacement Key audi a3 key fob (racingfans.com.au)
Composite Door Repair Near Me Tools To Improve Your Daily Life
Composite Door Repair Near Me Trick Every Person Should Know composite door repair (Pearline)
SEO Software For Small Business’s History Of SEO Software For Small
Business In 10 Milestones Search Engine Optimization Software
What Is Fabric Corner Sofa Beige’ History? History Of Fabric Corner Sofa Beige legend classic back fabric corner sofa
(Tommy)
15 Startling Facts About Programing Car Keys That You’d Never Been Educated
About Reprogramming Car Key (Naturalbookmarks.Com)
10 Things Everyone Hates About Renault Captur Key car locksmith Near me
17 Reasons To Not Avoid Crypto Live Casino live Casino crypto (gordonstiles09.livejournal.com)
A Provocative Remark About Cribs best rated cribs [Dina]
5 Laws To Help The Truck Accidents Lawyer Industry commercial truck accident lawyers
We recommend exploring the best quotes collections: Loved Quotes From Great People
What NOT To Do When It Comes To The Cheap Cot Bed Industry mini Cotbed
Anal Toy For Sale Explained In Fewer Than 140 Characters best anal plug for women (Melisa)
We recommend exploring the best quotes collections: Being In Love Quotes From Great People
How Ford Key Became The Top Trend On Social Media ford kuga key fob (Lillie)
5 Laws That Can Benefit The Double Glazed Windows
Near Me Industry Fit
A Provocative Remark About Window Hinges Repair Replacement Hinges (http://Www.Longisland.Com)
Undisputed Proof You Need Automotive Locksmith Key Programming Key Programmer
15 Up-And-Coming Bristol Door Panels Bloggers You Need To
Watch upvc window hinge repair near me
Private ADHD Assessment Near Me Tools To Enhance Your Everyday Life private adhd Assessment edinburgh cost
The Reason Pragmatic Slot Experience Is So Beneficial In COVID-19
프라그마틱 슬롯 환수율
Why No One Cares About Citroen C3 Key Replacement citroen Berlingo van key replacement
Mesothelioma attorneys specialize in asbestos
lawyer [minecraftcommand.science] litigation, which includes lawsuits and claims against trust
funds. They must understand complex laws of the state and national legal requirements to successfully process these types of claims.
What Mystery Box Could Be Your Next Big Obsession? mystery box online opening (Elsie)
20 Asbestos Attorneys Websites Taking The Internet By Storm mesothelioma lawyers (Steve)
“Ask Me Anything,” 10 Answers To Your Questions About Best Cot Newborn Cot Bed
Why Adult Adhd Assessment Near Me Is Still Relevant In 2023 How do Adults get Assessed for Adhd
Five Killer Quora Answers To Affordable Cots
affordable Cots
What’s The Good And Bad About Sports Toto Near Me 메이저사이트 바록가기 – Britney,
We recommend exploring the best quotes collections: Loved One Quotes From Great People
What Subaru Car Keys Experts Would Like You To Learn subaru Impreza key replacement cost
See What Crypto Thrills Casino Tricks The Celebs Are Utilizing crypto thrills casino (Lesli)
5 Must-Know Audi Car Key Techniques To Know For 2023 audi smart
key replacement (Leandro)
10 Electric Fireplace Wall Mounted Tricks All Experts Recommend fireplace
stove (bezmotora72.ru)
What Are The Reasons You Should Be Focusing On The Improvement Of
Organic SEO Agency seo marketing agency
10 Unexpected Fabric 2 Seater Sofas Tips Fabric 2 Seater Sofas Sale
10 Things Everybody Has To Say About Electric Wall Mounted Fire
Electric Wall Mounted Fire Mirror Fireplace Wall
7 Easy Secrets To Totally Doing The Patio Door Repair Company patio door repair company Near Me
A An Overview Of Saab 9-3 Key Replacement From Start To Finish saab 9-3 key fob replacement – Lucile –
10 Things That Everyone Doesn’t Get Right Concerning Audi A1 Key Replacement audi car key – http://www.Youtube.com,
Mesothelioma cases can be a bit complicated and can involve multiple defendants.
A reputable Asbestos Law
firm has an experienced team of experts who will know how to deal with all
defendants involved in a case.
I Lost My Car Keys Honda Strategies From The Top In The
Business how to program honda car key fob
5 Killer Quora Answers To Accident Injury Attorneys Near Me Accident Injury Attorneys Near Me
What Is Upvc Doors Birmingham? Heck Is Upvc Doors Birmingham?
Composite Door Installer Birmingham
If you wish for to take a good deal from this piece of writing then you have to apply
these techniques to your won web site.
I love it when individuals come together and share thoughts.
Great website, stick with it!
Guide To Small Patio Gas: The Intermediate Guide In Small Patio Gas small patio gas (Bessie)
10 Failing Answers To Common Double Glazing Cambridgeshire Questions
Do You Know Which Ones? Window mechnism Repair
How Pragmatic Ranking Its Rise To The No. 1 Trend In Social Media 프라그마틱 카지노
Greetings from California! I’m bored at work so I decided to check
out your website on my iphone during lunch
break. I really like the information you provide here and can’t
wait to take a look when I get home. I’m amazed at
how quick your blog loaded on my phone .. I’m not even using WIFI, just 3G ..
Anyways, awesome blog!
Saab Car Key Replacement Tools To Help You Manage Your Daily
Lifethe One Saab Car Key Replacement Technique Every Person Needs To Know saab Car key
What’s The Job Market For 2 Seat Fabric Sofa Professionals?
2 Seat fabric sofa
5 Killer Quora Answers To Infant Cot Bed infant Cot bed
5 Killer Quora Answers On Large Chest Freezers Uk chest freezers Uk
The Complete Guide To Renault Megane Key Card Replacement renault trafic
replacement Key (Bookmarkstore.download)
The 10 Most Terrifying Things About Beans To Coffee Machine Beans To Coffee Machine
Nine Things That Your Parent Teach You About Daftar
Akun Togel Resmi daftar akun togel resmi (gm6699.com)
What You Must Forget About Making Improvements To Your
Fold Away Treadmill health And fitness
Hi there to all, because I am truly keen of reading this weblog’s post to be updated daily.
It includes good data.
Swedish Massage 오피
The Time Has Come To Expand Your Emergency Locksmith Charges Options Locksmith Emergency service
The 10 Most Scariest Things About Asbestosis Asbestos Mesothelioma Attorney mesothelioma attorney
10 Quick Tips About Free Standing Electric Fireplace freestanding fireplace
The Most Hilarious Complaints We’ve Been Hearing About Mazda Replacement Key mazda 2 car key replacement (Monika)
Appreciating the hard work you put into your blog and detailed information you offer.
It’s nice to come across a blog every once in a while that isn’t the same unwanted rehashed information. Wonderful
read! I’ve bookmarked your site and I’m including your RSS feeds to my Google account.
Guide To Composite Door Scratch Repair: The Intermediate Guide To Composite
Door Scratch Repair composite Door scratch repair
Are you ready for a thrilling new challenge? Visit ovounblocked.me to experience the upgraded version of ovounblocked.me This latest update brings enhanced gameplay, smoother controls, and exciting new features, making it the ultimate destination for Ovo fans. Website: https://ovounblocked.me/
Howdy very nice web site!! Man .. Beautiful
.. Amazing .. I will bookmark your blog and take the
feeds additionally? I’m glad to find so many useful information here within the put
up, we need work out extra techniques in this regard, thank you
for sharing. . . . . .
That is very interesting, You are an overly skilled blogger.
I’ve joined your rss feed and sit up for searching for more of your excellent post.
Also, I have shared your web site in my social networks
This is very interesting, You’re a very skilled blogger.
I’ve joined your rss feed and look forward to seeking more of your great
post. Also, I’ve shared your web site in my social networks!
10 GSA SER Strategies All The Experts Recommend google
5 Killer Quora Answers On GSA SER Done For You gsa ser done for you
GSA SER Review Tips To Relax Your Daily Life GSA SER Review Trick That Every Person Should Learn Gsa
ser review (clinfowiki.win)
Your way of explaining all in this post is actually
good, all be able to without difficulty be aware of it, Thanks a lot.
Excellent post. Keep writing such kind of info on your
page. Im really impressed by it.
Hello there, You have done an excellent
job. I will definitely digg it and individually recommend to my friends.
I’m sure they will be benefited from this site.
Guide To English Pornstars: The Intermediate Guide On English
Pornstars english Pornstars
There’s certainly a great deal to find out about this topic.
I love all of the points you have made.
Say “Yes” To These 5 GSA SER List Tips gsaser
Hello there! This post couldn’t be written any better!
Reading this post reminds me of my old room mate! He always kept chatting about this.
I will forward this page to him. Fairly certain he will have a good read.
Thank you for sharing!
I’ll right away clutch your rss feed as I can not find your email subscription link or newsletter
service. Do you have any? Please permit me know in order that I may subscribe.
Thanks.
I’m not sure where you’re getting your info,
but great topic. I needs to spend some time learning more or understanding more.
Thanks for fantastic info I was looking for this information for
my mission.
excellent put up, very informative. I ponder
why the other experts of this sector do not realize this. You must continue your writing.
I’m sure, you’ve a huge readers’ base already!
5 Laws Everyone Working In Cheap Double Pushchair Should Know stroller double; Micheline,
Diese Seite
Hi there! Would you mind if I share your blog with my facebook group? There’s a lot of folks that I think would really appreciate your content. Please let me know. Many thanks
The History Of Boot Mobility Scooters mobility scooter portable car
boot folding lightweight (Azucena)
9 . What Your Parents Taught You About Car Key Fob Programming Near Me car key fob Programming near me
Bandar Togel Terpercaya Tools To Make Your Everyday Lifethe Only Bandar Togel Terpercaya Trick Every Person Should Know bandar togel terpercaya
How Adding A Audi Advanced Key To Your Life Can Make All The Difference Nearby
Do You Think Best Crypto Online Casinos Ever Be The King Of The World?
casino Games crypto
The 10 Scariest Things About Double Buggy 3 Wheels double buggy 3 wheels (longisland.com)
I do consider all the ideas you’ve offered on your post.
They’re really convincing and will definitely work. Still, the posts are very short for beginners.
May just you please lengthen them a little from next time?
Thank you for the post.
Find Out What Adhd Assessment The Celebs Are Making Use Of how to get An adhd assessment
The 10 Most Terrifying Things About Single Seat Buggy For Sale single seat buggy
Expert Advice On Porsche Macan Key Programming From An Older
Five-Year-Old Porsche Car Key Usb
7 Easy Tips For Totally Moving Your Porsche Spare Key
porsche cayenne replacement Key cost, telegra.ph,
Who’s The Top Expert In The World On Truck Accident Lawsuits?
semi truck wreck lawyer (Misty)
The Top Reasons People Succeed In The Saab 93 Key Fob Replacement Industry saab key fob replacement (Luigi)
10 Factors To Know About Auto Folding Mobility Scooter You Didn’t Learn At School auto folding scooter
See What Single Cot Bed Teak Wood Tricks The Celebs Are Using single cot bed Teak wood
See What Best Cots Uk Tricks The Celebs Are Using Best Cots Uk
Responsible For A Trucking Accidents Attorney Budget?
10 Ways To Waste Your Money Truck driver attorney
8 Tips For Boosting Your Crypto Casino Sites Game crypto casino games
Five Killer Quora Answers On Conservatories In Eastleigh Conservatories in Eastleigh
10 Tell-Tale Symptoms You Need To Know Before You Buy Fireplace Surrounds Marble Fireplace
5 Laws Anyone Working In Repair Double Glazing Should Know double
glazing repair – fakenews.win,
Quality articles is the important to be a focus for the people to pay a visit the web page,
that’s what this website is providing.
See What GSA Search Engine Ranker Services Tricks The Celebs Are Using gsa Search engine Ranker services
What’s The Job Market For Skoda Kodiaq Key Professionals Like?
skoda kodiaq key (cameradb.review)
What To Do To Determine If You’re Prepared For
Electric Wheelchair 25 Stone low cost Electric wheelchair
15 Secretly Funny People Work In Audi Key Audi q7 Replacement key
A Peek Into Key Repair Near Me’s Secrets Of Key Repair Near Me key Repair shop
“The Ultimate Cheat Sheet For Attorney For Asbestos mesothelioma attorney, Aisha,
Best Automatic Folding Mobility Scooter Uk Tools To Help You Manage Your Daily Life Best Automatic Folding Mobility Scooter Uk Trick Every Person Should Know Best Automatic Folding Mobility Scooter Uk
What Is Truck Crash Attorney? History Of Truck Crash Attorney commercial truck accident
attorney (browne-puggaard.mdwrite.Net)
The Reason Truck Accident Attorneys Is So Beneficial For COVID-19 semi truck Lawyers
Why Is Everyone Talking About Handle For Double Glazed Window Right Now
window handle repairs (Leonora)
10 Meetups About Bmw Replacement Key Fob You Should Attend reprogram
This Is How 3 Wheeled Buggies Will Look Like In 10 Years Time 3
wheel infant Stroller (http://www.play56.net)
Why Assessments For Adhd Is Fast Becoming The Hottest Trend Of 2023 how to get a adhd assessment (Hellen)
Upvc Windows Near Me Tools To Ease Your Daily Lifethe One Upvc Windows Near Me
Trick That Should Be Used By Everyone Learn Upvc Windows Near Me
The Full Guide To Subaru Car Keys subaru remote key
How To Get More Results From Your Key Replacement For Car
Car key replacement price
11 “Faux Pas” That Are Actually Acceptable To Make With
Your Car Key Spares Car Remote Key Replacement
How To Train Your Cat To Use A Window Cat Flap window Cat flap
The 10 Most Terrifying Things About Electric Fire Media
Wall electric Fire media wall
This Is The Advanced Guide To Jaguar Replacement Key Fob Jaguar Xj Replacement Key
A Look Into The Future What Will The Door Fitters Milton Keynes Industry Look Like In 10 Years?
Lock and Key milton keynes
Think You’re Ready To Start Crawley Window Repair? Take This Quiz aluminum Window Repair
What’s The Current Job Market For Audi Replacement Car Keys Professionals?
audi replacement car keys
The 10 Scariest Things About Best British Pornstars Best British Pornstars
Repair Double Glazing Window Tools To Ease Your Everyday Lifethe Only Repair Double Glazing Window Technique
Every Person Needs To Know repair Double glazing window
10 Things That Your Family Taught You About Heavy
Duty Electric Wheelchair Uk Heavy Duty Electric Wheelchair Uk
Rollators For Seniors Tools To Ease Your Daily Lifethe One
Rollators For Seniors Trick That Every Person Should Be Able To Rollator
What a stuff of un-ambiguity and preserveness of valuable
knowledge on the topic of unexpected feelings.
8 Tips To Up Your Double Glazing Milton Keynes Game Lock Replacements Milton Keynes
5 Killer Quora Answers On Best Crypto Casino Usa Best crypto casino USA [Rafael]
2 Seater Fabric Sofas Uk Techniques To Simplify Your
Daily Lifethe One 2 Seater Fabric Sofas Uk Technique
Every Person Needs To Know 2 Seater fabric sofas uk
How Can A Weekly Program A Car Key Project Can Change Your Life how to
program a car key (telegra.Ph)
15 Gifts For The Case Battle Lover In Your Life Case battle csgo
Don’t Buy Into These “Trends” Concerning Online Mystery Box mystery box opening Online
15 Latest Trends And Trends In Volkswagen Car Key
how to lock volkswagen without key (netvoyne.ru)
12 Companies Are Leading The Way In Nissan Juke Key Fob Nissan Keys
What’s The Job Market For ADHD In Adults Self Assessment Professionals?
Adhd In Adults Self Assessment; Minecraftcommand.Science,
15 Top Pinterest Boards From All Time About Asbestos Mesothelioma Lawsuit Mesothelioma attorneys
Why Nobody Cares About Replacement Bmw Key prices
Corner Electric Fireplace With Mantel Tools To Ease Your Daily Life Corner Electric Fireplace With
Mantel Trick That Every Person Should Learn corner electric fireplace with mantel
The Best Crypto Casino Online Tricks To Transform Your Life
best crypto Casino online
It’s Enough! 15 Things About Togel4d We’re Tired Of Hearing Togel Singapore
What’s The Job Market For ADHD Assessment For Adults London Professionals?
adhd assessment for adults
When some one searches for his essential thing, so he/she needs to
be available that in detail, thus that thing is maintained over here.
Composite Door Replacement Lock Tips To Relax Your Daily Life Composite Door Replacement Lock Trick Every
Individual Should Know Composite Door replacement lock
20 Rising Stars To Watch In The Nissan Key Fob Replacement Industry nissan car keys
The One Sash Window Refurbishment Mistake That Every Newbie Makes sash windows repair
The 10 Scariest Things About Best Quality Bunk Beds Best Bunk Bed
It’s going to be ending of mine day, however before ending
I am reading this impressive piece of writing
to increase my know-how.
A Step-By Step Guide For Choosing Your Pragmatic Slot Tips 프라그마틱 슈가러쉬
5 Killer Quora Answers To Accidents Attorney Near Me Accidents Attorney Near Me
Lamborghini Diablo Key Tips From The Best In The Business Lamborghini key replacement
An In-Depth Look Into The Future What’s The Togel4d Industry Look Like In 10
Years? situs togel online
15 Reasons You Must Love Bromley Door Panels window lock repair Near me
15 Great Documentaries About Woodburning Stove small modern Wood
stoves; rutelochki.ru,
The Most Worst Nightmare Concerning Private Psychiatrist
South Wales Bring To Life best private psychiatrist
london (Wilton)
11 “Faux Pas” That Are Actually Okay To Create Using Your
ADHD Medication prescribe Adhd medication
The Most Worst Nightmare About Preventive Measures For Depression Be Realized seasonal Depression treatment
10 Wrong Answers To Common Private Adhd Assessment Questions Do You Know The Right Ones?
adhd Assessment questions
The Best Maxi Cosi Car Seat Stroller Tricks To Make A Difference In Your Life best
maxi cosi car seat (liftrecord1.werite.net)
Why Nobody Cares About Bioethanol Freestanding
Fire bioethanol Freestanding Fireplace
What You Should Be Focusing On Improving Tilt And Turn Window Tilt And Turn Window Repair Near Me
Why No One Cares About Nissan Juke Key Replacement Car key repair
Cars Locksmiths Techniques To Simplify Your Everyday Lifethe Only Cars Locksmiths Technique Every
Person Needs To Learn cars locksmiths (Tressa)
20 Fun Facts About Pragmatic Slots Free Trial 프라그마틱
The No. One Question That Everyone Working
In ADHD Medications Should Be Able Answer Over the counter adhd medication uk
Don’t Buy Into These “Trends” Concerning Lawyer For Car Accidents best lawyer for
car accident (Felicitas)
Five Killer Quora Answers On Accidents Attorney Near Me Accidents Attorney near me
17 Reasons To Not Be Ignoring Audi Car Keys Replacement Shop
A Reference To Key Fob Repair From Beginning To End car key Fob repair service
5 Killer Quora Answers To Media Wall And Fireplace Media wall and fireplace
Adding A Composite Door Cat Flap composite Door cat flap
What’s The Reason You’re Failing At Locksmith Car Near Me car lock.smith (Jamel)
5 Killer Quora Answers On Double Glazing Window
Repair Double glazing Window repair
12 Companies Setting The Standard In Togel4d situs togel online – Situstotoslot51053.blogerus.com,
Bioethanol Fireplace: 10 Things I’d Love To Have Known Earlier wooden Fireplaces
Nine Things That Your Parent Teach You About Bmw Replacement Car Keys Bmw replacement car key
17 Reasons Why You Shouldn’t Ignore Coffee Beans
Coffee Machine bean to cup espressomaschine
It’s a shame you don’t have a donate button! I’d without a doubt donate to this brilliant
blog! I guess for now i’ll settle for bookmarking and adding your RSS feed
to my Google account. I look forward to new updates and will share this site with my Facebook group.
Talk soon!
The Reasons Toyota Car Key Replacement In 2023 Is The Main Focus Of All People’s
Attention. 2023 Toyota Rav4 Replacement Key Fob Uk
10 Tips For Quickly Getting Kia Replacement Key
Uk kia optima key replacement cost (Shiela)
How To Make An Amazing Instagram Video About Space
Saving Treadmill With Incline does treadmill incline burn more calories (Eugenio)
Bifold Door Replacement Tips To Relax Your Daily Life Bifold Door Replacement Trick
That Everybody Should Learn Bifold door replacement (Securityholes.science)
You’ll Never Guess This Lawyer Injury Accident’s Secrets lawyer injury Accident
Why Double Glazing Crawley You’ll Use As Your
Next Big Obsession? Glass replacement near Me
The Most Pervasive Problems In Smart Car Key automotive locksmith near me
What’s The Reason You’re Failing At Crypto Coin Casino
best crypto casino; Gabriel,
The One Private Psychiatrist Assessment Mistake That
Every Beginner Makes private psychiatrist consultation cost,
Patti,
3 Wheeled Travel System Is The Next Hot Thing In 3 Wheeled Travel System 3 Wheel Stroller With Car Seat
What’s The Job Market For Pellet Stoves Modern Professionals?
pellet stoves modern (Jacquetta)
You’ll Never Guess This Where To Buy Arabica Coffee
Beans’s Tricks where to buy arabica coffee beans
The Most Advanced Guide To Best Cot Bed Baby Cots On Sale
What Is Local Accident Attorneys? History Of
Local Accident Attorneys In 10 Milestones Accident Lawyer
Five Killer Quora Answers On Small L Shaped Settee small l shaped settee
Five Killer Quora Answers On Chimineas Clay Chimineas clay
Why No One Cares About Mesothelioma Compensation Mesothelioma Attorney
Five Killer Quora Answers To Daftar Situs Togel
Daftar Situs Togel
Watch Out: How Audi Key Is Gaining Ground And How To Respond audi a1 key fob
(daojianchina.com)
You’ll Be Unable To Guess Chesterfield Grey Corner Sofa’s Tricks Chesterfield grey corner sofa
15 Trends To Watch In The New Year Auto Key Locksmith
24 hour auto locksmith (Kent)
20 Misconceptions About Audi Spare Key: Busted audi key Replacement cost
8 Tips To Up Your Cutting Car Key Game Cheap Car Key cutting
4 Dirty Little Secrets About The ADHD Diagnosis
Industry Private adhd.diagnosis
You’ll Never Guess This Handles And Hinges’s Tricks Handles And Hinges
10 Apps To Help Manage Your L Shaped Couch l shaped sofabed (intern.Ee.aeust.edu.tw)
Five Killer Quora Answers On Replacement Key For Audi A3
replacement key for audi a3 (Charolette)
Guide To Daftar Akun Togel Resmi: The Intermediate Guide To Daftar Akun Togel Resmi daftar Akun togel resmi
10 Facts About Couch And Loveseat That Will Instantly
Set You In A Positive Mood small sofa bed couch
What’s The Job Market For Car Key Repair Shop Near Me Professionals?
Car Key Repair – Telegra.Ph –
15 Presents For Your Treadmills Sale Lover In Your Life treadmills for sale (Hildegard)
20 Insightful Quotes About Mobile Car Key Cutting Mobile Key Cutting
Why You Should Concentrate On The Improvement Of
Car Key Repair Near Me broken car key repair near me, Lamar,
7 Tips About Nissan Qashqai Key That No One Will Tell You Replacement key for nissan Juke; holman-tuttle.federatedjournals.com,
The 12 Best Composite Door Repair Accounts To Follow On Twitter Composite door repairs near me
Why People Are Talking About Pragmatic Demo
This Moment 프라그마틱 슬롯
I will right away seize your rss feed as I can’t find your email subscription hyperlink or newsletter service.
Do you have any? Please let me recognize in order
that I could subscribe. Thanks.
What’s The Current Job Market For Accident Injury Attorneys Near
Me Professionals? Accident Injury Attorneys Near Me
10 Things We Hate About Car Door Key Lock Repair car Key duplication
Buzzwords De-Buzzed: 10 Other Methods For Saying Togel Sydney
situs togel online
Cat Flap Fitters window cat Flap
Why Install A Double Glazing Cat Flap? double Glazing cat flap
9 Things Your Parents Teach You About Situs Togel Online situs Togel online
Nine Things That Your Parent Taught You About Programmed Car Keys programmed car Keys
The 10 Most Terrifying Things About Mitsubishi Galant Key Replacement mitsubishi galant key replacement (Kirsten)
Win79 game bai truc tuyen chat luong va uy tin den tu Singapore cung cap nhieu the loai : Mau binh, tien len dem la, ban ca… cung voi nhieu khuyen mai hap dan. win79bet.link
You’ll Be Unable To Guess Large 2 Seater Fabric Sofa’s Benefits large 2 seater
fabric sofa (Erna)
One Key Trick Everybody Should Know The One Programing Car Keys Trick Every Person Should Be Aware Of mobile car Key programming near me
10 Things That Your Family Teach You About Wall
Mounted Electric Fireplace With Mantel Ideas Wall Mounted Electric Fireplace With Mantel Ideas
9 Things Your Parents Taught You About Locksmith Near Me For Home
Locksmith near me For Home
15 Gifts For The Case Battle Lover In Your Life Cs Case Battle
Don’t Believe These “Trends” Concerning 50 50 Fridge Freezer Integrated Frost Free 50 50 refrigerator
What’s The Reason You’re Failing At Folding Wheelchair best folding wheelchair – Alicia,
Good day! I know this is kind of off topic but I was wondering
if you knew where I could find a captcha plugin for my comment
form? I’m using the same blog platform as yours and I’m
having difficulty finding one? Thanks a lot!
Searching For Inspiration? Check Out Car Accident Compensation Claim auto car accident lawyers
See What Crypto Thrills Casino Tricks The Celebs
Are Making Use Of crypto thrills casino (Lenore)
Why Everyone Is Talking About Skoda Replacement
Key Cost Uk Right Now Skoda Kodiaq Key Replacement
Replacement Audi Car Key’s History Of Replacement Audi Car Key In 10
Milestones audi replacement key Cost uk (0lq70ey8yz1b.com)
20 Best Tweets Of All Time About ADHD Private Diagnosis Private ADHD assessment Bristol Cost
The Best Mystery Boxes Techniques To Rewrite Your Life
mystery box open game (Xxh5gamebbs.uwan.com)
What’s The Job Market For Best Crypto Casino 2024
Professionals? Best crypto casino 2024
Windows Seal Replacement Techniques To Simplify Your Daily Lifethe One Windows Seal Replacement Trick Every Individual Should Know windows Seal replacement
20 Fun Details About Truck Accidents Attorney truck accident attorney
5 Qualities That People Are Looking For In Every New Ferrari Key ferrari lost key
The History Of Key Programmers Program Car Key
The One Asbestos Attorneys Mistake Every Beginner Makes Mesothelioma Lawyers
2 In 1 Stroller Car Seat Tools To Improve Your Everyday Lifethe Only 2 In 1 Stroller Car Seat Trick Every Individual Should Be Able To 2 in 1 Stroller Car Seat
ADHD Assessment Private Tools To Ease Your Daily Life
ADHD Assessment Private Trick That Should Be Used By Everyone Learn adhd assessment private
Guide To Accident Injury Attorney: The Intermediate Guide Towards Accident Injury Attorney accident injury attorney
10 Key Factors To Know Seat Car Key Replacement You Didn’t Learn In School seat leon replacement key
You’ll Never Guess This Citroen Remote Key Replacement’s Tricks Citroen Remote Key
Replacement (Ashworth-Hartvigsen.Technetbloggers.De)
The Secret Secrets Of Pragmatic Recommendations 프라그마틱 정품 사이트 (linkingbookmark.Com)
Item Upgrade: What Nobody Is Talking About Item upgrader
The Biggest Problem With Adhd Assessment For Adults And How You Can Resolve It Cheap Adhd Assessment
5 Commercial Truck Accident Lawyer Projects That Work For
Any Budget Truck accident attorneys
A Journey Back In Time: How People Talked About Audi Key 20 Years Ago audi remote key (zenwriting.net)
10 4 Wheel Electric Mobility Scooter Meetups You Should Attend mobility 4 wheel scooters (Dallas)
10 Wrong Answers To Common Toto Macau Questions Do You Know The Right Answers?
situs Toto
You’ll Never Guess This Togel4d Login’s Benefits togel4d login –
Elena,
12 Facts About Online Mystery Box To Make You Think Smarter
About Other People best one time mystery box (stairways.wiki)
A An Overview Of French Door Fridge From Start To
Finish french door retro fridge
How To Create An Awesome Instagram Video About Mini Cot Beds
best cot bed (Royce)
10 Times You’ll Have To Know About Fix Window Handle
upvc window handles near me (postheaven.net)
20 Things You Need To Be Educated About Private ADHD Assesment adhd assessment For adults private
Link Togel Tools To Make Your Daily Life Link
Togel Trick That Every Person Must Learn Link Togel – Designbean78.Werite.Net,
14 Common Misconceptions About Wall Electric Fireplace Wall Fire electric
Is Tech Making Mini Cooper Key Better Or Worse? replacement car key mini cooper (Clair)
Ask Me Anything: 10 Responses To Your Questions About Pragmatic Slot Recommendations 프라그마틱 체험
Five Killer Quora Answers On Real Leather Sofa Real leather sofa
What’s Everyone Talking About Machines Espresso Right Now bean to cup espresso machine
What’s The Job Market For Fold In Treadmill Professionals? Fold In Treadmill [http://Www.80Tt1.Com]
Ten Window Repair Near That Will Actually Help You Live
Better upvc window Repair near Me
The Reasons You’re Not Successing At Upvc Door Hinge types of upvc door hinges
Where Will Audi Replacement Car Keys Be One Year From Now?
Audi Car key replacement Cost
What’s Next In Bmw Replace Key lost key Bmw
Watch Out: What Electric Stove Is Taking Over
And How To Stop It electric heating stove (Minerva)
11 Strategies To Completely Defy Your Honda
Key Replacement Near Me Replacement honda civic key Fob
What Experts In The Field Of Car Key Programing Want You To Be Able To car key programmers
Hey there I am so glad I found your weblog, I really found you
by mistake, while I was researching on Google for something else, Nonetheless I am here now and
would just like to say many thanks for a fantastic post and a all round thrilling blog
(I also love the theme/design), I don’t have time to read through it all at the moment but I have bookmarked it and also added your RSS feeds,
so when I have time I will be back to read more, Please do keep up the superb work.
You’re About To Expand Your Replacement Audi
Car Key Options Audi Tt Replacement Key
Bed Cot Design Wooden Tools To Improve Your Everyday Lifethe Only Bed Cot Design Wooden Trick That Should Be Used By Everyone Be Able To
bed Cot design wooden
What’s Next In Car Door Key Lock Repair Door Lock Car Repair
5 Killer Quora Answers On Bi Folding Door Repair Near Me bi
folding door repair (marvelvsdc.faith)
5 Killer Quora Answers On Asbestosis Asbestos Mesothelioma Attorney Mesothelioma Attorney
The Sage Advice On Retro White Fridge Freezer From A Five-Year-Old under counter retro fridge Freezer
10 Myths Your Boss Has Concerning Peritoneal Mesothelioma Not Caused By Asbestos Mesothelioma attorney
The Most Effective Advice You’ll Receive About ADHD Test For Women adhd with women (Eddy)
The Top Reasons Why People Succeed In The Crypto Live Casino Industry Crypto Casino Sites (http://Www.Diggerslist.Com)
Five Killer Quora Answers To Sofas 2 Seater Fabric Sofas 2 seater fabric
5 Laws That Will Help The Daftar Akun Togel
Resmi Industry Bandar Toto
5 Reasons To Be An Online Mobile Automobile Locksmith And 5 Reasons
Why You Shouldn’t mobile automobile locksmith near me (Florian)
Why People Are Talking About Midi Bed Today double midi bed
What Is Mystery Box’ History? History Of Mystery Box online mystery
box opening (Vonnie)
The Top Companies Not To Be Follow In The Butt Plugs Online Industry butt plug sex
20 Myths About ADD Treatments For Adults: Busted symptoms of untreated adhd (Hunter)
Why All The Fuss Over Integrated French Style Fridge Freezer?
French Style Fridge Freezer Reviews Uk
Who Is The World’s Top Expert On Private
Testing For ADHD? Adhd Assessment For Adults Private
9 Lessons Your Parents Taught You About Babiie Pram Babiie pram
11 Strategies To Completely Defy Your Asbestos Attorney Mesothelioma Lawsuit
10 Online Cryptocurrency Casino Tricks Experts Recommend Online Crypto Casino
What’s The Current Job Market For Best Cot Newborn Professionals?
best cot Newborn
Why You Should Be Working On This Car Accident Claim Car Accident Lawyer Best
Who Is Responsible For An Crypto Game Casino Budget?
12 Tips On How To Spend Your Money crypto games Casino
5 Killer Quora Answers To Bi Folding Door Repair Near
Me bi folding door repair near me
A Peek Inside The Secrets Of Best Crib best crib for newborn [Connie]
10 Misconceptions That Your Boss May Have About Locksmiths Near Me
Auto Locksmiths Near Me Auto emergency Locksmith
These Are The Most Common Mistakes People Make When Using
Car Replacement Key Cost lost car key replacement near me
15 Gifts For Your Best Cryptocurrency Casino Lover In Your Life Bitcoin Casino
The No. 1 Question Anyone Working In Upvc Windows Repair Should Be Able To
Answer Repair Upvc Windows
10 Startups That’ll Change The Treadmill That Folds Up
Industry For The Better Treadmill foldable
Mesothelioma From Asbestos Techniques To Simplify
Your Everyday Lifethe Only Mesothelioma From Asbestos Trick
Every Individual Should Learn mesothelioma Lawsuit
3 Reasons Your Key Lexus Is Broken (And How To Repair It)
lost
Could Long Couch With Chaise Be The Answer For 2023’s
Challenges? double chaise sectional – Zelda –
10 Things We All Are Hating About Best Sex Machine sex toy machines
Mesothelioma Attorney Tools To Streamline Your Daily Lifethe One Mesothelioma Attorney Trick That
Everyone Should Learn mesothelioma
20 Things That Only The Most Devoted Mental Health Assessment Fans Are Aware Of Early Help Assessment Mental Health (Menwiki.Men)
20 Myths About ADHD Treatment Adults: Debunked Treatment For Adhd In Adults
Very quickly this web site will be famous amid all blog users, due to it’s fastidious articles
5 Clarifications On Window Repair Near upvc window repair near me
Seven Reasons To Explain Why Ferrari Spare Key Is Important ferrari Key Fob Replacement
What’s The Current Job Market For Best G Spot Dildo Professionals Like?
best g spot dildo
10 Quick Tips About Pragmatic Free Slots 프라그마틱 무료스핀
See What Treatment For Panic And Anxiety Attacks Tricks The Celebs Are Using treatment for Panic And anxiety attacks
The 10 Most Infuriating Subaru New Key-Related FAILS
Of All Time Could’ve Been Prevented locked keys in subaru forester (Willie)
You’ll Never Be Able To Figure Out This Walking Rollator With Seat’s Tricks Walking Rollator With Seat
Five Things You Don’t Know About 3 Wheel Rollators adjustable Rollator
15 Top Twitter Accounts To Learn More About Retro Fridge Freezer Sale Fridge Freezer Retro Style
2 Seater Fabric Sofas Uk Tools To Make Your Daily Life 2 Seater
Fabric Sofas Uk Trick That Should Be Used By Everyone Learn 2 seater fabric
sofas uk (Dianne)
The 10 Scariest Things About Fold Up Wheelchairs
Fold up wheelchair
20 Resources That Will Make You Better At Uk Private Psychiatrist private psychology
near me (Angelica)
20 Things You Should ASK ABOUT Bunk Beds For Children Before You Buy Bunk Beds For Children buy Bunk Beds
9 Things Your Parents Taught You About ADHD Assessment For Adults Edinburgh Adhd Assessment For Adults Edinburgh
This Is How Spare Honda Key Will Look In 10 Years Time honda spare key replacement
Why You Should Not Think About How To Improve Your Automotive Locksmith Key Programming Automotive key programmer
What’s The Current Job Market For Double Glazing Near Me Professionals?
Double glazing near me
Why You Should Focus On Enhancing Toto4d Toto Online Terbaik
What The 10 Most Worst Upvc Replacement Window Handles FAILURES Of All Time Could
Have Been Prevented Online Upvc windows
Why Nobody Cares About Saab Key Lost saab keys
17 Reasons To Not Ignore Crypto Coin Casino Casino Game crypto
See What Top Rated Cots Tricks The Celebs Are Using top rated Cots
25 Surprising Facts About Remote Key Fob Repair remote key fob repairs (Tobias)
What Is Trucking Accidents Lawyers? History Of Trucking Accidents Lawyers big truck accident lawyers
What Freud Can Teach Us About Bean To Cup Coffee Machine
Bean To Cup Coffee Maker
20 Resources To Make You More Efficient With Anonymous Crypto Casino online crypto casino (Arnette)
You’ll Be Unable To Guess Lawyer Injury Accident’s Benefits lawyer injury accident
What Experts On Accident Lawyers In Miami Fl Want You To Know?
accident lawsuit
You’ll Never Guess This Crypto Wild Casino’s Tricks Crypto Wild Casino
Wooden Cot And Bed Tools To Improve Your Daily Life Wooden Cot And
Bed Trick That Every Person Must Be Able To wooden cot and bed (Lovie)
20 Resources That’ll Make You Better At Commercial Truck Accident Attorney semi truck accident lawyer near me – Thorsten,
Are You Responsible For The Car Key Cutters Near Me Budget?
12 Ways To Spend Your Money automotive Locksmith
Every weekend i used to pay a quick visit this web
page, because i want enjoyment, for the reason that this this web site conations actually pleasant funny stuff
too.
9 Lessons Your Parents Taught You About Patio Door Glass Repair Patio Door Glass Repair
Online Crypto Casino: A Simple Definition best online crypto casino (Thomas)
The Hidden Secrets Of Sofa Sale Clearance sectional sale
Now That You’ve Purchased Pragmatickr … Now What? 프라그마틱 사이트 – Raymundo,
The Next Big Event In The Truck Lawyers Near Me Industry truck accidents lawyer – Orville,
A Look At The Secrets Of Mesothelioma Asbestos Claim mesothelioma lawyer
(Mabel)
The Ultimate Guide To Double Glazing Shops Near Me Double Galzed windows
Nissan Juke Key Replacement: A Simple Definition nissan Navara d40 key replacement
What’s The Job Market For Best Folding Treadmill For Small
Space Professionals? best folding Treadmill for Small space
Mobility Scooter For Sale Near Me: The History Of Mobility Scooter For Sale Near
Me In 10 Milestones Motorised Mobility Scooters For Sale
The Best Indoor Scooters Gurus Are Doing Three Things Electric Mobility Scooter Uk
Speak “Yes” To These 5 Tread Mills Tips treadmill
What’s The Job Market For Sleeper Sofas For Sale Professionals Like?
Sleeper Sofas For Sale
How To Outsmart Your Boss On Key Reprogramming Car Key Programer
Five Killer Quora Answers To Mesothelioma Compensation mesothelioma compensation (Dokuwiki.stream)
Is Cut Car Keys The Best Thing There Ever
Was? key Duplication
The Next Big Thing In Double Glazing Hinges Window Door Repairs Locks Glass Hinges
Are You Confident About Squirting Dildo Shop? Try This Quiz best sex Toy to make you squirt
Now That You’ve Purchased Car Key Replacements …
Now What? Car Key Fob Replacement
5 Killer Quora Answers To Audi A4 Key Replacement Audi a4 key replacement
Smart Aluminium Tilt And Turn Windows Tips To Relax Your Daily Lifethe One Smart Aluminium Tilt And Turn Windows Trick That Everybody Should Learn smart Aluminium tilt and turn windows
Five Killer Quora Answers On Crypto Casino Coins Crypto Casino Coins
What ADHD Adult Treatment Experts Want You To Be Educated When Adhd Goes Untreated
10 Subaru Impreza Key-Related Projects That Stretch Your Creativity how much To replace subaru key
Getting Tired Of Mesothelioma Attorney? 10 Inspirational Sources That
Will Bring Back Your Passion mesothelioma law firms (Madison)
A Trip Back In Time The Conversations People Had About Best Sex
Machine 20 Years Ago Sex Machinee
The Reason Why Crypto Casino Games Is Everyone’s Obsession In 2024 Crypto casino slots
[writeablog.net]
How Misted Double Glazing Repairs Became
The Hottest Trend In 2024 misted double glazing repairs Near me
How To Find The Perfect Mesothelioma Claim On The Internet Mesothelioma Litigation
Five Killer Quora Answers On Find Accident Attorney accident Attorney
Five Killer Quora Answers To Wall Mount Electric Fireplace
With Mantel wall mount Electric fireplace with mantel
7 Simple Tricks To Totally Doing The 1kg Coffee Beans 1kg coffee beans Price uk
Ten Porsche Car Key Myths You Should Not Share On Twitter porsche Macan Key
13 Things About Situs Togel Online You May Not Have Known bandar Toto
15 Gifts For The Ultralight Electric Wheelchair Lover In Your Life electric
bariatric wheelchair [Andra]
The Top Baby Cot Bed The Gurus Are Using 3 Things cot beds – topspeed.lv,
The People Nearest To Renault Key Have Big Secrets To Share nearest
You’ll Never Guess This Bifold Door Repairs Near Me’s Tricks Bifold door repairs near me
It’s The Online Crypto Casino Case Study You’ll
Never Forget Crypto Casino Online
Mazda 3 Key Tools To Simplify Your Everyday Life 2017 mazda 3 key fob programming; Raina,
15 Gifts For The Car Keys Cutting Near Me Lover In Your Life automotive Key cutting
Nine Things That Your Parent Teach You About Ethanol Fireplaces Ethanol Fireplaces
The Mesothelioma Asbestos Claims Awards: The Top, Worst, Or Most Bizarre Things We’ve Seen Mesothelioma attorney
The 10 Most Scariest Things About Car Attorneys Near Me car attorneys (Chad)
10 Apps That Can Help You Control Your Asbestos
Mesothelioma mesothelioma Lawyers [stairways.Wiki]
The Hidden Secrets Of Audi A1 Key audi keyless Entry
13 Things About Mesothelioma And Asbestos You May Never
Have Known Mesothelioma Lawsuits
The Most Hilarious Complaints We’ve Heard About
Mental Health Assessment mental state assessment
Question: How Much Do You Know About Mercedes Spare Key Cost?
replacement mercedes Keys
Could Volkswagen Key Fob Be The Key To Achieving 2024?
volkswagen key Fob replacement near me; willysforsale.com,
The Most Worst Nightmare Concerning Strollers Get Real Convertible Strollers
Solutions To Issues With Pragmatic Free Trial Slot Buff 프라그마틱 무료체험 메타
[Armanir.Com]
Nine Things That Your Parent Teach You About Volkswagen Key Fob
Replacement volkswagen key Fob replacement
Why Everyone Is Talking About Mesothelioma Attorney Assistance Right Now Mesothelioma Lawyers
What’s The Current Job Market For Chesterfield Sofa L Shape Professionals Like?
chesterfield sofa l shape
The Little-Known Benefits To Lightweight Foldable Electric Wheelchairs
electric Wheelchairs foldable lightweight
How Adding A Glass Window Replacement Near Me To Your Life Will Make
All The Change window glass replacement near me (peatix.com)
Need Inspiration? Look Up Window Companies Milton Keynes
key cutting In milton Keynes
5 Killer Quora Answers To Best Crypto Casino Usa
Best crypto casino USA
What Is The Heck What Is Car Locks Smith? Carkey Locksmith (Whitebookmarks.Com)
Best Sex Machine: What Nobody Has Discussed sex machine for sale [bookmarkfeeds.Stream]
15 Best Documentaries On Fire Place For Media Wall electric media wall Fire
10 No-Fuss Methods For Figuring Out Your Legit Crypto Casino casinos that accept crypto
(Roxanne)
An intriguing discussion is worth comment. I do believe that you should publish more about this topic, it might not be a taboo subject but usually people don’t discuss these subjects.
To the next! Cheers!!
10 Electric Treadmill Incline That Are Unexpected treadmill electric folding; Lane,
What’s The Job Market For Keyrepair Professionals?
keyrepair
How Much Do Car Keys Programming Experts Earn? program Car Keys
14 Cartoons About Key Audi That’ll Brighten Your Day near By
How Window And Door Doctor Can Be Your Next Big Obsession window and Door doctor near me
The 10 Most Scariest Things About Modern Leather Couch pure leather Sofa
This Is The Good And Bad About Mesothelioma Attorney mesothelioma lawyer (Pansy)
7 Things About Wall Mount Electric Fireplaces
You’ll Kick Yourself For Not Knowing Wall Fireplaces Electric, 80Aakbafh6Ca3C.рф,
13 Things About Renault Key Card Replacement Near Me You
May Not Have Known ignition
5 Killer Quora Answers To Foldable Flat Treadmill Foldable flat treadmill
What’s The Current Job Market For Composite Door
Replacement Keys Professionals Like? Composite door Replacement keys
A How-To Guide For Crypto Online Casino From Start To Finish Casino with crypto
What’s The Current Job Market For Big Clay Chiminea Professionals Like?
big clay chiminea
10 Wrong Answers To Common Fiat Key Questions: Do You
Know Which Ones? programmers
A Peek Inside The Secrets Of Renault Kadjar Replacement Key Renault Kadjar Key Card Replacement Cost (Postheaven.Net)
You’ll Never Be Able To Figure Out This Sliding Patio Door Repair Service’s
Tricks sliding patio door repair service
How To Explain Fridge Freezer French Doors Uk To Your
Boss integrated french Door fridge freezer uk
10 Startups That Are Set To Revolutionize The
Treatment For ADD Industry For The Better non medication treatment for Adhd adults
5 Killer Quora Answers To Crypto Casino Coins crypto casino coin
The 10 Most Terrifying Things About Situs Toto Login situs toto login (bookmarklethq.com)
10 Tell-Tale Warning Signs You Need To Get A New Crypto Casino Us Crypto
casino usa [Google.co.Ao]
What Is Realistic Masturbators For Men And Why Is Everyone Speakin’ About It?
best mastubator for men
14 Cartoons About For Sale Mobility Scooters To Brighten Your Day small mobility Scooter for Sale
9 Lessons Your Parents Teach You About Upvc Double Glazed Sash Windows Double Glazed Sash Window
5 Must-Know Practices For Audi A4 Spare Key In 2023 audi remote key (Theresa)
8 Tips To Increase Your Pragmatic Demo Game 프라그마틱 슬롯 사이트
The Biggest Issue With What Causes Mesothelioma Other Than Asbestos And How You Can Resolve It mesothelioma attorneys – Lucienne,
You’ll Never Guess This Best Rated Pellet Stoves’s Tricks
best rated pellet stoves
Ten Things You’ve Learned In Kindergarden To Help You Get Started With Leather Chesterfield Sofa Grey Leather Chesterfield
Who Is Glass Repair And Why You Should Care patio door glass Repair;
guidekidney7.bravejournal.net,
The 3 Most Significant Disasters In Velvet Sectional Sofa
The Velvet Sectional Sofa’s 3 Biggest Disasters In History sectional sofa sale
Ten Things You Learned In Kindergarden That Will Help You With Double Glazed Windows Manchester door and window installation manchester
What’s The Reason You’re Failing At Private ADHD Assessment private adhd assessment oxford
10 Things You’ve Learned About Preschool That’ll Help You With Suzuki Key Suzuki Sx4 Key Replacement
The Biggest Sources Of Inspiration Of Coffee To Bean Machine Bean-To-Cup Coffee Machines
A reputable mesothelioma lawyer will examine your work or military background to determine where and when asbestos lawsuit [Janette]
exposure is likely to have occurred. They can also provide information on different types of compensation.
We recommend exploring the best quotes collections: Lovely Quotes From Great People
Forget Accident Injury Lawyers: 10 Reasons Why You Don’t Really
Need It accident attorney
Everything You Need To Know About Link Togel Dos And Don’ts Link togel Resmi
Ten Blue Leather Chesterfield That Will Change Your Life velvet chesterfield sofa, Hildegarde,
How To Outsmart Your Boss Bi-Fold Door Hinges
aluminium window Hinge Replacement – articlescad.com,
10 Facts About How Much Is A Private ADHD
Assessment That Will Instantly Put You In A Good Mood private adhd assessment cost uk
We recommend exploring the best quotes collections: I Love You Quotes From Great People
25 Shocking Facts About Adhd Assessment Adult Adhd Assessment Cost
10 Things You Learned In Kindergarden To Help You Get Started With Electric Log Burner Fire Realistic electric wood Stove
See What Window Repair Luton Tricks The Celebs Are Utilizing window repair
The Best Accident Injury Lawyers Near Me Tricks To Transform Your Life best accident injury lawyers (Marcella)
Best ADHD Medication For Adults With Anxiety And Depression Tips To Relax Your Daily Lifethe One Best ADHD Medication For Adults With Anxiety And Depression Trick That Every Person Must
Learn best adhd medication for adults With anxiety
What’s The Job Market For Lamborghini Svj Key Professionals?
lamborghini Svj key
You’ll Be Unable To Guess Patio Doors Repair Near Me’s Tricks patio doors Repair near me
10 Mistaken Answers To Common Daftar Situs Togel Questions Do You Know The Right Answers?
Togel Hongkong
Nine Things That Your Parent Taught You About Leather Sofa With Chaise Leather Sofa
See What Automatic Folding Mobility Scooter Uk Tricks The Celebs Are Making Use Of Automatic Folding Mobility Scooter Uk
Why How Much Does It Cost To Replace A Porsche Key Is Fast Becoming The Most Popular Trend In 2023 porsche key replacement cost uk
Guide To Double Glazing Windows Repair: The Intermediate Guide The Steps To Double Glazing Windows Repair
double glazing windows repair
How Much Can Upvc Door Repair Experts Make? Upvc door repair service near me
Enough Already! 15 Things About Get Diagnosed With ADHD We’re Tired Of Hearing Adhd diagnostic process
Train Accident Lawsuit: What Nobody Is Talking About Attorney truck Accident
How To Build A Successful Toyota Aygo Key Replacement Even If You’re Not Business-Savvy toyota car remote key replacement,
Ned,
It’s The Myths And Facts Behind Accident Lawyers In Miami Fl Accident Lawsuits
Don’t Make This Mistake On Your Car Accident Case car
injury attorney near me (Melvina)
See What Modern Electric Fires Freestanding Tricks The Celebs Are Using
electric Fires freestanding
Guide To Sectional With Chaise And Sleeper: The Intermediate Guide Towards Sectional With Chaise And Sleeper sectional With Chaise And Sleeper
Guide To Espresso Machine Sale: The Intermediate Guide The Steps
To Espresso Machine Sale Espresso Machine Sale
20 Insightful Quotes On Mobile Auto Locksmith Near
Me automotive locksmith key fob
You’ll Be Unable To Guess Togel Resmi Indonesia’s
Secrets togel resmi indonesia – bbs.airav.asia,
It’s The Complete Cheat Sheet On Truck Accident Lawyers For Hire
semi Truck wreck lawyer
What’s The Job Market For Car Key Repair Shop
Near Me Professionals? car
How Much Do Replace Window Sashes Experts Make? sash window restoration Near me
Drip Filter Coffee Machine 101 The Ultimate Guide For Beginners Kitchenaid Drip Coffee Maker
The Best Advice You Can Receive About Mesothelioma Asbestos Lawyer mesothelioma lawyer
There Are A Few Reasons That People Can Succeed
Within The Upvc Door Hinge Types Industry upvc window hinges types
Best Folding Treadmill: What’s No One Has Discussed treadmill Folding treadmill
The People Closest To Pragmatic Tell You Some Big Secrets 프라그마틱 슬롯 환수율
5 Killer Quora Answers To Online Cots online cots [gdchuanxin.Com]
See What Audi A3 Key Replacement Tricks The Celebs Are Using audi a3 Key
10 Healthy Top Accident And Personal Injury Lawyers Habits accident Lawsuit
The Most Negative Advice We’ve Ever Been Given About Media Fireplace Wall ezee glow 50 celestial built in media wall
electric fire (Clemmie)
You’ll Be Unable To Guess Fold Up Travel Wheelchair’s Tricks fold up travel wheelchair
10 Fundamentals About Fabric Recliner Corner Sofa You Didn’t Learn At School large fabric Corner sofa Uk
What’s The Job Market For Cheap Cot Beds Professionals Like?
cheap cot beds
5 Laws Everybody In Treatments Of ADHD Should Know treatment for inattentive adhd in adults, telegra.Ph,
What Is It That Makes Trucking Lawyers So Popular?
Construction truck accident lawyer
9 Lessons Your Parents Teach You About Double Glazed Window
Suppliers Near Me double Glazed window suppliers near Me
[Privatehd.Org]
Why You Must Experience Nissan Key Fob At The Very Least Once In Your Lifetime Nissan Qashqai Keys Locked In Car
Electric Garden Patio Heater Tools To Improve Your Daily Life Electric Garden Patio
Heater Trick That Should Be Used By Everyone Learn Electric garden patio heater
15 Documentaries That Are Best About Crypto Slots Casino cryptoslots Casino
My programmer is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the
costs. But he’s tryiong none the less. I’ve been using WordPress on various websites for about a year
and am nervous about switching to another platform.
I have heard fantastic things about blogengine.net.
Is there a way I can transfer all my wordpress content into it?
Any help would be really appreciated!
A An Instructional Guide To Audi Convenience Key From Beginning To End audi Remote key
5 Killer Quora Answers To Upvc Door Hinge Repair Near Me Door Hinge Repair (Funsilo.Date)
Today, I went to the beach with my children. I found a sea
shell and gave it to my 4 year old daughter and said “You can hear the ocean if you put this to your ear.” She placed the shell to her
ear and screamed. There was a hermit crab inside and it pinched her ear.
She never wants to go back! LoL I know this is completely off topic
but I had to tell someone!
5 Killer Quora Answers To Accident Attorney Near Me accident attorney near me (Linda)
10 Facts About Mystery Boxes That Can Instantly Put You In The Best Mood open online mystery boxes
Trucking Accidents Attorneys Isn’t As Tough As You Think Commercial truck accident lawyer –
Elektroavto.lv,
10 Wrong Answers To Common Window Repair Birmingham Questions Do You Know Which Answers?
Shop front repairs birmingham
It can take decades for the disease to develop from the initial exposure, and symptoms usually don’t appear until the
cancer is in an advanced stage.
My blog post: Asbestos
The History Of Car Accident Compensation Claims Attorney For Car Crash
Smart Car Key Replacement Tools To Enhance Your Day-To-Day Life Smart Car Key Programming Near Me
20 Trailblazers Leading The Way In Nissan Juke Key Fob Nissan Replacement Keys
How To Create An Awesome Instagram Video About Private Psychiatrist Edinburgh private Psychiatrist online
It’s The Ugly Truth About Double Glazing Repair Milton Keynes
door repairs milton keynes – franks-dreier-2.technetbloggers.de –
Watch Out: What Asbestos Cancer Lawyer Mesothelioma Settlement Is Taking Over
And What You Can Do About It mesothelioma lawsuits (lentz-morrow-4.blogbright.net)
8 Tips To Increase Your Folding Rollator Game ultra lightweight rollator walker (Emilie)
9 Lessons Your Parents Teach You About Pushchairs Prams pushchairs Prams
You’ll Never Guess This Window Repair Near Me’s Secrets window repair near me
The Myths And Facts Behind Replacement Mazda Key mazda key copy (Vanessa)
10 Wrong Answers To Common LG Refrigerator Uk Questions Do You
Know The Correct Answers? Lg Fridge Freezer
The 10 Most Terrifying Things About Car Replacement Key Cost car replacement key cost
I’m gone private adhd assessment Right to choose say to my little brother, that he should also
pay a visit this web site on regular basis to get updated from latest news.
15 Up-And-Coming Pragmatic Image Bloggers You Need
To Keep An Eye On 프라그마틱 무료
How Titration ADHD Adults Its Rise To The No. 1 Trend On Social Media private adhd
medication titration (Sung)
You’ll Never Be Able To Figure Out This ADHD Assessment For Adults
Uk’s Tricks Adhd Assessment For Adults Uk [Timeoftheworld.Date]
The 9 Things Your Parents Teach You About Electric Patio Heater Hanging electric Patio heater hanging
Accident Injury Lawyers Near Me Tools To Make Your Daily Lifethe One Accident Injury Lawyers Near
Me Trick Every Individual Should Know Accident injury lawyers near me
You’ll Never Be Able To Figure Out This Leather 2 Seater Chesterfield
Sofa’s Secrets 2 seater chesterfield; bookmarkangaroo.com,
It’s The Ugly Facts About All Crypto Casinos
Crypto Casino’s
15 Best Mystery Boxes Bloggers You Must Follow best mystery boxes
See What Window Hinge Repairs Tricks The Celebs Are Using window hinge repairs (Lazaro)
See What Rollators Walkers Tricks The Celebs Are Utilizing rollators walkers
These Are The Most Common Mistakes People Make With Audi
Q7 Car Key Replacement audi Replacement key fob
How To Get More Benefits Out Of Your Foldable Electric Treadmill Folding Electric Treadmill
How To Determine If You’re Ready To Go After Auto Accident Compensation Claims car Collision lawyers near Me
Patio Door Seal Replacement: 11 Thing You’ve Forgotten To Do window seal replacement Cost
10 Unexpected Auto Lawyer Near Me Tips Attorneys Car Accident
What’s The Job Market For Tilt And Turn Window Not Closing Professionals?
tilt and turn window not closing properly
The Three Greatest Moments In Car Replacement Key History Car
Replacement Keys (Images.Google.Com.Gt)
How Much Do Asbestos Cancer Lawsuit Lawyer Mesothelioma Experts Earn? Mesothelioma lawsuits
Ten Repair Car Keys That Really Change Your Life repair car keys
You’ll Never Be Able To Figure Out This Upgrade
Item’s Tricks upgrade item – images.google.bi
–
It’s The One Single Pushchair Sale Trick Every Person Should Know Single pushchairs
There’s A Reason Why The Most Common Auto Key Locksmith Debate Isn’t As Black
And White As You Might Think how much does an auto locksmith cost
uk – Tera –
Howdy! This is my 1st comment here so I just wanted to give
a quick shout out and say I genuinely enjoy reading through your blog
posts. Can you recommend any other blogs/websites/forums that deal
with the same topics? Thanks for your time!
20 Best Tweets Of All Time About Replacement Key For Skoda
Fabia Skoda car key replacement cost [lovewiki.faith]
10 Facts About Audi Car Key Replacement That Will Instantly Put You In A Positive Mood
Audi spare key Cost
10 Steps To Begin Your Own Double Glazed Glass Replacement Business replacement Glass for a Door
4 Dirty Little Details About The Auto Locksmith Industry automotive locksmith programming near me (Danielle)
10 Program A Car Key Tips All Experts Recommend car Key reprogram Near me
The Fold Up Electric Wheelchair Success Story You’ll Never Remember fold Up electric wheelchairs
What’s The Current Job Market For Electric Fireplace Mantel Only Professionals Like?
electric fireplace mantel only (Cory)
Five Killer Quora Answers On Integrated Combi Fridge Freezer Integrated Combi Fridge Freezer
Tandem Double Stroller: 10 Things I’d Like To Have Learned Earlier
double stroller With Bassinet (Livebookmark.stream)
Why Adhd Assessment Adult Still Matters In 2023 Adult adhd assessment [minecraftcommand.science]
Why You Should Focus On Improving Double Bed Bunk Beds
double bed bunk With desk
You’ll Never Be Able To Figure Out This Lawyer Injury Accident’s Secrets lawyer Injury Accident
Window Repair Near Me Tools To Make Your Everyday Lifethe Only Window Repair Near Me Trick
Every Individual Should Be Able To Window repair near me
A Provocative Rant About Fire Suite realistic Electric fire suites
15 Things Your Boss Wished You Knew About Bean Cup Coffee Machine bean cup coffee machines
10 Basics About Case Opening Battles You Didn’t Learn In School
Case Opening Battle Csgo
The Most Successful Pragmatic Free Trial Meta Experts Have Been Doing Three Things 프라그마틱 데모
The 9 Things Your Parents Teach You About Compact Travel Scooters Compact travel scooters
10 Wrong Answers For Common Asbestos Mesothelioma Compensation Questions:
Do You Know The Right Ones? mesothelioma attorney (http://www.kaseisyoji.com)
Patio Doors Repairs Explained In Less Than 140 Characters sliding patio doors repair
10 Things Everybody Hates About Audi Key Fob
Replacement Audi Key Fob Replacement replacement Audi key Cost uk
11 Ways To Completely Redesign Your Key Replacement Toyota 2010 toyota corolla key
For Whom Is Crypto Games Casino And Why You Should Care casino with crypto
5 Upvc Doors Aylesbury Projects For Every Budget windows close to me
Pragmatic Free Slots Tips From The Top In The Industry 프라그마틱 정품 확인법
Windows And Doors Bedford’s History History Of Windows And Doors Bedford replacement upvc Windows bedford
5 Killer Quora Answers On Locksmith Ignition Replacement Cost Locksmith ignition replacement cost
The No. 1 Question Everyone Working In How To Repair Broken Car Key Must Know How To Answer key repair shops near Me (http://Www.dermandar.com)
Quiz: How Much Do You Know About Cot Bed? best Cots
15 Top Mesothelioma Attorney Bloggers You Need To Follow Top mesothelioma attorney
What The 10 Most Stupid Accident & Injury Lawyers FAILS Of All Time Could Have Been Prevented
lawyer near me accident (Jacquie)
The Reasons Wood Burning Stove Outdoor Is More Difficult Than You Think best wood burning Stove
How Much Do Audi Advanced Key Experts Earn? Audi a1 key fob
You’ll Never Be Able To Figure Out This Audi Lost Key’s Benefits audi lost key
What Pragmatic Slots Free Will Be Your Next Big Obsession 무료 프라그마틱,
Coy,
Why We Enjoy Wood Burners (And You Should Also!) wood burning stoves for sale near me
4 Dirty Little Secrets About Modern Chiminea And The Modern Chiminea Industry chimineas
Your Family Will Be Grateful For Getting This Mystery Box online mystery box Opening
Mesothelioma occurs when the linings that surround the
body’s organs, including the lungs, stomach,
reproductive organs and the heart, develop out of control.
my site :: asbestos Legal
The 10 Scariest Things About Patio Door Repair Service Near Me Patio
Door Repair Service Near Me (http://Www.Annunciogratis.Net)
9 Things Your Parents Taught You About Electric Lightweight Wheelchair
electric lightweight wheelchair (Chara)
How To Tell If You’re Ready For Volvo Key Replacement how do i get a replacement volvo key
20 Private ADHD Assessment Websites Taking The Internet By Storm Private ADHD assessment
Brighton cost (Deb)
Cots 4 Tots Tools To Make Your Everyday Lifethe Only Cots
4 Tots Trick Every Individual Should Be Able To Cots 4 tots
What Experts Say You Should Be Able To car Key locksmith Near me
The 10 Scariest Things About Accident Attorneys Near
Me accident attorneys near me (Maryjo)
The 10 Most Infuriating Replacement Panels For Upvc
Doors Failures Of All Time Could Have Been Prevented
upvc back Door panel (pattern-wiki.win)
Ten Accident Injury Attorneys That Really Make Your Life Better accident injury attorneys (Gertrude)
Why Truck Accidents Lawyer Near Me Is Fast Increasing To Be The Hot Trend For 2023 commercial truck accident Attorneys (Voprosi-otveti.ru)
The 10 Most Scariest Things About Sash Window Locks With Key Sash Window Locks With Key
Nine Things That Your Parent Teach You About Upvc Patio
Door Repairs Upvc Patio Door Repairs
The Best Place To Research Private ADHD Test Online private adhd assessment medway (enbbs.instrustar.com)
You’ll Never Guess This Couch L Shaped Sofa’s Tricks couch l shaped Sofa
Could Lightweight Foldable Electric Wheelchair Be The Key To 2023’s Resolving?
Foldable lightweight Electric Wheelchair
Through Wall Cat Flap through wall cat flap (Major)
See What How Much Is A Private ADHD Assessment UK Tricks The Celebs Are
Utilizing how much Is a private adhd assessment uk
12 Facts About Locksmith For Cars To Make You Look Smart Around Other People mobile key Smith For cars
10 Websites To Help You To Become An Expert In Double Glazing Repairs
Cambridge window Lock repairs
You’ll Never Guess This Truck Lawyers Near Me’s Tricks Truck Lawyers
11 Ways To Completely Sabotage Your Wall Mount Fireplace electric wall hung fireplace (Danilo)
See What Top Rated Cots Tricks The Celebs Are Using
Top rated cots
5 Killer Qora’s Answers To Situs Togel Terpercaya situs toto togel (http://www.demilked.com)
The Ultimate Guide To Audi A4 Key Replacement audi a4 replacement key
You’ll Be Unable To Guess Togel4d Login’s Tricks togel4d login
Upvc Repairs Near Me Tools To Streamline Your Everyday Lifethe Only Upvc Repairs Near Me Trick Every Individual Should Learn upvc repairs Near me (lakechild66.werite.net)
Who Is Vauxhall Insignia Key And Why You Should Consider Vauxhall Insignia Key vauxhall insignia key replacement (Timothy)
Upvc Doors Birmingham: The Good, The Bad, And The Ugly
Window Glaziers Birmingham
The 10 Most Terrifying Things About Patio Sliding Door Repair Near Me patio sliding door repair near
me (Judy)
17 Reasons Not To Avoid Case Battle cs Case Battle (itkvariat.com)
My relatives always say that I am killing my time here at web, but I know I am
getting familiarity all the time by reading such nice posts.
Guide To Situs Togel Dan Slot Terpercaya: The Intermediate Guide
Towards Situs Togel Dan Slot Terpercaya Situs Togel dan slot Terpercaya
Magnificent beat ! I wish to apprentice while you amend your
web site, how could i subscribe for a blog web site?
The account helped me a acceptable deal. I had been a little bit acquainted of this your broadcast offered bright clear idea
What Experts Say You Should Know How To Test Adhd In Adults – Marvelvsdc.Faith,
Seven Explanations On Why Media Wall Fireplace Is Important media wall fire
places (Bernadette)
Seven Reasons Why Best Accident Lawyers Is So Important Lawyer Near Me Accident
What Is Automatic Fold Up Mobility Scooter? History
Of Automatic Fold Up Mobility Scooter Automatic Fold Up Scooter
What’s The Job Market For Link Togel Professionals? Link Togel
10 Untrue Answers To Common Four Seater Chesterfield
Sofa Questions: Do You Know The Right Answers?
grey velvet chesterfield Sofa
Heya! I just wanted to ask if you ever have any problems with hackers?
My last blog (wordpress) was hacked and I ended up losing many months of hard work due to no backup.
Do you have any methods to stop hackers?
You’ll Never Be Able To Figure Out This Double Glazed Windows Repair Near
Me’s Benefits Double glazed windows repair
20 Irrefutable Myths About Folding Treadmills With Incline:
Busted foldable treadmill (Kendrick)
Ten Door Glass Repairs That Really Make Your Life Better door Glass repairs
Five Killer Quora Answers On 3 Wheel Stroller Cheap 3 Wheel Stroller
Heya i am for the first time here. I found this board and
I find It truly useful & it helped me out a lot. I hope to give something back and
help others like you aided me.
The 10 Most Scariest Things About Repair Bifold Door Top Pivot Repair Bifold Door Top Pivot
10 Meetups About Togel4d You Should Attend toto4d (Swen)
What’s up, everything is going well here and ofcourse every one is sharing information, that’s genuinely good, keep up writing.
60 Inch Tall Electric Fireplace With Mantel Tools To Streamline Your Daily
Lifethe One 60 Inch Tall Electric Fireplace With Mantel Trick That Should
Be Used By Everyone Be Able To tall electric Fireplace with mantel,
delphi.Larsbo.org,
The Benefits Of Auto Accident Law Firm Near Me At A Minimum, Once In Your Lifetime attorney car accident near me
A Brief History Of Private Psychiatrist Diagnosis History Of Private Psychiatrist Diagnosis How to find a private psychiatrist uk
10 Websites To Help You Develop Your Knowledge About Sectional With Chaise chaise sectional
In a mesothelioma case, the lawyers will want to examine all of a victim’s medical records.
These records will include victim’s test results and diagnosis, which
is usually confirmed with lab tests, such as an X-ray,
CT scan, or MRI.
Also visit my web site – asbestos compensation (Wikimapia.Org)
You’ll Never Guess This Aluminium Patio Door Repairs’s Tricks aluminium patio door repairs
How To Outsmart Your Boss With Fabric Corner Couch Left Hand Fabric Corner Sofa
The 3 Greatest Moments In Best Folding Wheelchairs History foldable wheelchair for elderly
10 Websites To Help You Learn To Be An Expert In Getting A Diagnosis For ADHD Adhd Symptoms
You’ll Never Guess This Treadmill Sale UK’s
Secrets treadmill sale uk
Ten Cheap Electric Wheelchairs That Really Change Your Life cheap electric Wheelchairs
You’ll Never Be Able To Figure Out This L Shaped Couch Sofa’s
Secrets l Shaped Couch Sofa
The statute of limitations is a legal term which specifies the maximum period
during which families and victims can file a lawsuit against asbestos claim,
Celia,.
The law of the state sets this limit, which differs from state to state.
Your Family Will Be Grateful For Getting This Double Glazed Sash Windows Double glazed sash windows cost
What’s The Job Market For Best Rated Folding Treadmill Professionals Like?
best Rated Folding Treadmill
2 In 1 Car Seat And Pram Tools To Ease Your Daily Life 2 In 1 Car Seat And Pram Trick That Every Person Should Know 2 in 1 car seat and pram – Carley –
What’s The Job Market For Bi-Fold Door Hinges Professionals?
bi-fold door Hinges
15 Top Car Accident Attorney Bloggers You Must Follow Top Car accident attorney
Why We Enjoy Hinges (And You Should Also!) double glazing Hinge Replacement
What’s The Current Job Market For Replace Double Glazing Seals Professionals?
Replace double glazing Seals
Why Who Repairs Sliding Patio Doors Is Your Next Big Obsession sliding patio door repairs
15 Of The Most Popular Pinterest Boards Of All Time About Replacement Double Glazing
Glass Only sash
Guide To L Shaped Sofa Leatherette: The Intermediate Guide Towards L Shaped Sofa Leatherette L shaped Sofa leather
Ten Reasons To Hate People Who Can’t Be Disproved Train Accident Case semi truck accident lawyers Near me
Where Can You Get The Most Reliable Pragmatic Genuine Information? 프라그마틱 슈가러쉬, Betty,
14 Cartoons On Pragmatic Free Trial Slot Buff To Brighten Your Day 프라그마틱 무료체험 – bookmarkrange.Com,
Could Auto Accident Claim Compensation Be The Key To
Dealing With 2022? Car Accident Injury Attorneys
Good day! This is my first visit to your blog!
We are a team of volunteers and starting a new initiative
in a community in the same niche. Your blog provided us beneficial information to work on. You have done a marvellous job!
Hey are using WordPress for your site platform?
I’m new to the blog world but I’m trying to get started
and create my own. Do you require any coding knowledge to
make your own blog? Any help would be greatly appreciated!
Check Out The Three Wheel Pushchair Tricks That The Celebs Are Making Use Of 3 wheel baby Stroller
A Comprehensive Guide To Pragmatickr. Ultimate Guide To
Pragmatickr 프라그마틱 무료체험 메타
“The Hinge Repair Plate Awards: The Most, Worst, And Weirdest Things We’ve Ever Seen door hinge repair (Ronny)
10 Myths Your Boss Is Spreading About Hiring Auto Accident Attorney lawyer car accident near me (Rudy)
7 Effective Tips To Make The Most Of Your Pragmatic Demo
프라그마틱 환수율 (Olivebookmarks.Com)
10 Life Lessons We Can Take From Upgrade Item item upgrades (Kattie)
The 3 Greatest Moments In Cheap Double Buggy History Thule Double Stroller
From Around The Web 20 Amazing Infographics About Cheap Sectional Couch Velvet Sectional Couch
Do You Think Good Accident Lawyers Be The
Next Supreme Ruler Of The World? good accident lawyers near me [Shawn]
One Best Auto Accident Lawyers Success Story You’ll
Never Believe lawyers near me car accident, Darci,
The 10 Scariest Things About Sofas L Shape sofas l
shape – sofasandcouches17188.p2Blogs.Com,
The Reasons Lightest 3 Wheel Stroller Is Harder Than You Imagine
3 wheel stroller for running – Ray,
Are You Getting The Most Out The Use Of Your Upvc Door Lock Repairs Near Me?
Upvc Scratch Door Repair
You’ll Be Unable To Guess All Terrain Folding Electric Wheelchair Uk’s Secrets All Terrain Folding Electric Wheelchair Uk (Asiavalley8.Bravejournal.Net)
The Next Big Trend In The Mesothelioma Attorneys Near
Me Industry mesothelioma Lawyer
What’s Everyone Talking About Link Togel This Moment Link togel resmi
(advicebookmarks.com)
15 Gifts For The Auto Accident Lawyer For Hire Lover In Your Life Lawyers for car accident near Me
11 “Faux Pas” That Are Actually Okay To Make With Your Mesothelioma Asbestos Claims mesothelioma attorneys – Rob –
You’ll Be Unable To Guess Black Composite Door Scratch Repair’s Secrets Black composite door scratch repair
Guide To Replacement Window Hinges: The Intermediate Guide
In Replacement Window Hinges Replacement Window Hinges
15 Of The Most Popular Pinterest Boards Of All Time About Item Upgrade Item Upgrader
Foldable Wheelchairs For Sale Tools To Ease Your Daily Life Foldable Wheelchairs For Sale Trick
That Should Be Used By Everyone Know foldable Wheelchairs for Sale
A Sage Piece Of Advice On 3 Wheeled Rollator With Seat From An Older Five-Year-Old Indoor rollator
You’ll Never Guess This Misted Double Glazing Repairs’s Tricks Misted Double Glazing Repairs
What’s Holding Back The Bristol Door And Window Industry?
Window fitters Bristol
What’s The Fuss About Auto Accident Lawyers Near Me? Car Accident Lawyer No Injury
The 10 Most Terrifying Things About Situs Toto Login situs toto
login (yxzbookmarks.com)
A Complete Guide To Window And Door Doctor window and door doctor near me
See What Patio Glass Door Repair Near Me Tricks The Celebs Are Making Use Of Patio Glass Door Repair Near Me [Mckenna-Hanna.Blogbright.Net]
Guide To Injury Accident Lawyers: The Intermediate Guide In Injury Accident Lawyers
injury accident lawyers (Jeffry)
The 10 Most Scariest Things About 3 Wheeler
Stroller 3 wheeler Stroller
4 Dirty Little Details About Non Asbestos Causes Of Mesothelioma Industry Non Asbestos Causes Of
Mesothelioma Industry mesothelioma attorney – Ermelinda,
A Guide To Mesothelioma Settlement From Start To Finish mesothelioma legal (Mariano)
Five Killer Quora Answers On Best Travel Pushchair Travel Pushchair
15 Best Item Upgrades Bloggers You Need To Follow best Item upgrade
(maps.Google.no)
10 Life Lessons We Can Learn From Sleeper Couch Leather sleeper sofa (digitaltibetan.win)
15 Twitter Accounts That Are The Best To Discover Windows And Doors Harrow bifold doors harrow (Shawnee)
See What Situs Terpercaya Tricks The Celebs Are Making
Use Of situs terpercaya
Installing A Cat Flap In A UPVC Door Cost cat flap
Are You Responsible For An Attorneys Accidents Budget?
10 Unfortunate Ways To Spend Your Money accident lawyers (Lynn)
The Best Double Glazing Repair In Cambridge Is Gurus.
Three Things Double glazing seal repairs
20 Tips To Help You Be More Efficient At Couch Beds For
Sale New couch for sale [zanybookmarks.com]
Pragmatic Casino: The Good, The Bad, And The Ugly 프라그마틱 무료게임 –
Wallace –
What’s The Job Market For Link Togel Professionals Like?
Link Togel
Attorneys For Automobile Accidents Strategies From The Top In The Business attorney
near me car accident (Florentina)
You’ll Be Unable To Guess Accident And Injury Attorneys’s Tricks accident and injury attorneys (Camille)
Five Ramps For Wheelchairs Projects To Use For Any Budget Portable folding wheelchair Ramps
Guide To Situs 4d: The Intermediate Guide To Situs 4d Situs 4D
Mesothelioma attorneys specialize in Asbestos Lawsuit litigation including lawsuits and
claims against trust funds. They must understand complex laws of the state and national legal requirements to be able to successfully handle these kinds of claims.
Wisdom On Stained Glass Repair Near Me From An Older Five-Year-Old
double glass window repair
See What Two Seater Fabric Sofa Uk Tricks The Celebs Are Utilizing two seater fabric sofa uk (http://www.stes.tyc.Edu.tw)
10 Things Everyone Hates About Toto4d situs togel online
Fantastic goods from you, man. I have understand your stuff previous to and you are
just extremely excellent. I actually like what you have acquired here, certainly like what you are
saying and the way in which you say it. You make it entertaining and you
still take care of to keep it sensible. I cant wait to read much more from you.
This is actually a great site.
Get To Know You The Steve Jobs Of The Pragmatic Korea
Industry 프라그마틱 무료게임
9 Things Your Parents Taught You About Accident Injury Attorneys Near
Me accident injury attorneys
Everything You Need To Know About Upvc Double Glazed Windows upvc windows sale
The Most Pervasive Problems In Pragmatic Genuine 프라그마틱 슬롯 하는법
The 10 Scariest Things About Bi-Fold Door Repair bi-Fold door Repair
10 Pragmatic Demo Techniques All Experts Recommend 프라그마틱 무료체험 슬롯버프
14 Smart Ways To Spend Your The Remaining Non Asbestos Causes Of
Mesothelioma Budget mesothelioma attorney
Does Technology Make Accident Attorney Lawyer Better Or Worse?
Lawyer near me Accident
Cat Flap Double Glazing Cat flap double glazing
What Experts Say You Should Learn case battle cs go – Roslyn –
How To Make A Successful Truck Accident Instructions For
Homeschoolers From Home Big Truck accident Lawyers
Why You’ll Need To Learn More About Online Mystery Box the best mystery boxes
The 10 Most Terrifying Things About Pvc Window Hinges Pvc Window Hinges
8 Tips To Boost Your Upvc Door Panel With Cat Flap Game Upvc front door insert panels
See What Repair Upvc Windows Tricks The Celebs Are Using repair Upvc Window
Why Install A Double Glazing Cat Flap? Double Glazing Cat Flap
How Much Do Local Locksmith Experts Make? local Locksmiths Near Me
The Most Significant Issue With Double Glazing Window Handles And How You
Can Resolve It tilt and turn window handles
asbestos Lawyer – waugh-hein-2.blogbright.net – lawyers
are experts at seeking compensation on behalf of those suffering from asbestos-related
diseases. They will review your medical records, work
history and other information to find possible asbestos-related
exposure sources.
How To Survive Your Boss With Trucking Accidents
Attorneys Trucking Accident Lawyer Near Me
15 Best Accident Lawyer Near Me Bloggers You Must Follow best
accident lawyer near me (Carson)
Ten Accident Injury Attorneys That Really Make Your Life Better accident injury attorneys
Looking For Inspiration? Try Looking Up Car Accident Lawsuits Top rated car accident lawyers
From Around The Web From The Web: 20 Awesome Infographics About Upvc
Window Hinge upvc window hinge replacement (Shellie)
Guide To Accident Claim Lawyers: The Intermediate Guide To
Accident Claim Lawyers Accident Claim Lawyer
What’s The Job Market For Composite Door Replacement Keys Professionals Like?
composite door Replacement Keys
5 Killer Quora Answers On Conservatories In Eastleigh conservatories In eastleigh
How To Make An Amazing Instagram Video About Repair Upvc Door Frame how To repair upvc door
What’s The Current Job Market For Accidents Attorney Near Me Professionals Like?
accidents attorney near me (Veronica)
See What Mesothelioma Tricks The Celebs Are Utilizing
Mesothelioma
What’s Everyone Talking About Windows Repair This Moment double glazed window repairs near me
Guide To Upvc Windows And Doors Repairs: The Intermediate Guide On Upvc Windows And Doors Repairs upvc windows
and doors repairs (Margarito)
20 Fun Facts About Truck Accident Attorney Near Me Truck Injury Attorneys
10 Facts About Glass Repair Harrow That Make You Feel Instantly A Good
Mood double glazing window Repair
Why Nobody Cares About Mesothelioma Attorneys Mesothelioma claim
15 Gifts For The Bi-Fold Door Repair Lover In Your Life bi-fold door repairs near me
16 Must-Follow Instagram Pages For Car Accident Attorney Marketers best car crash Attorney
From the 1930s to the 1970s, Asbestos Settlement was
extensively employed in construction materials. It was used
as insulation for pipes, fireproofing products cements and plasters, automobile brakes and much more.
There Is No Doubt That You Require Tilt And Turn Window Adjustment tilt and turn windows adjustment
(Trisha)
Ten Auto Lawyers Near Me Products That Can Change Your Life Car accident Attorney
Let’s Get It Out Of The Way! 15 Things About Clearwater Accident Lawyer We’re Overheard Lawyer Accident Near Me
3 Ways The Mesothelioma Law Influences Your Life mesothelioma Compensation
A Delightful Rant About Upvc Window Repair double glazing upvc Windows
Replacement Lock For Composite Door Tools To Help You Manage Your Daily Life Replacement Lock
For Composite Door Trick That Everybody Should Be Able To Replacement Lock For Composite Door
A Cheat Sheet For The Ultimate On Top Accident Attorney Accident Injury
10 Things Everybody Gets Wrong About The Word “Homeowner Gas Safety Certificate” Safety certificates
You may be able bring a lawsuit in the event that you or someone
you love has been diagnosed with a disease related to asbestos case – Odessa,.
A mesothelioma lawyer will help you determine your options and begin the process.
10 Steps To Begin The Business You Want To Start Best Accident Injury Lawyers Business Lawyer Accident Near Me
A Provocative Remark About Accident Attorney lawyer for accidents near me
Train Accident Settlements It’s Not As Expensive
As You Think commercial truck accident attorneys; Bbs.nhcsw.com,
Landlord Gas Safety Certificate: The Good, The Bad,
And The Ugly landlord gas safety certificate
cost (Shavonne)
No matter if some one searches for his vital
thing, therefore he/she wishes to be available that in detail, therefore that
thing is maintained over here.
WOW just what I was searching for. Came here by searching for บอล สด
I needed to thank you for this good read!! I absolutely loved every bit of it.
I have got you book marked to check out new things you post…
Accident & Injury Lawyers 10 Things I Wish I’d Known Earlier Accident And Injury (Digitaltibetan.Win)
Compensation from an asbestos Lawsuit (stevens-allen-2.Federatedjournals.Com) can aid families
of patients pay for outstanding medical bills funeral expenses, income loss
as well as the pain and suffering of the past.
How To Create An Awesome Instagram Video About Car
Accident Attorneys car accident injury lawyers
9 Lessons Your Parents Taught You About Tilt And Turn Windows Aluminium tilt And turn windows aluminium
Guide To Accident Attorney Lawyer: The Intermediate Guide On Accident Attorney Lawyer
accident attorney lawyer (Alethea)
The 10 Most Terrifying Things About Accident Lawyers Gainesville Accident lawyers
(articlescad.com)
whoah this weblog is excellent i like reading your articles.
Stay up the great work! You already know, a lot of individuals are looking round
for this info, you could help them greatly.
What Is Misted Double Glazing And How To Utilize It?
Misted double glazing repairs [Underwood-hyde.thoughtlanes.net]
Five Killer Quora Answers On Car Accidents Attorneys car accidents attorneys; m1bar.com,
Are Mesothelioma Attorney The Same As Everyone Says?
mesothelioma law firms – Dannie –
Despite the fact that asbestos case (Bianca) usage declined in the 1970s, exposure this dangerous mineral may
cause life-threatening illnesses like mesothelioma.
I blog frequently and I genuinely appreciate your content.
The article has really peaked my interest. I’m going to
take a note of your site and keep checking for new information about once per week.
I subscribed to your Feed too.
You’ll Be Unable To Guess Accident And Injury Attorneys’s Tricks Accident And Injury Attorneys
How To Save Money On Asbestosis Asbestos Mesothelioma Attorney mesothelioma attorneys
(Alba)
Five Killer Quora Answers To Gas Safety Certificate UK gas Safety certificate uk
Car Accident Injury Lawyers Tips From The Best In The Industry lawyer near me For
car accident [http://www.nlvbang.com]
10 Tips For Asbestos And Peritoneal Mesothelioma That Are
Unexpected mesothelioma Lawsuit
I used to be able to find good info from your content.
The Unknown Benefits Of Asbestos Attorneys mesothelioma lawsuits,
Carmella,
7 Essential Tips For Making The Most Of Your Top Accident And Personal Injury Lawyers accident Lawsuit (selfless.wiki)
I enjoy what you guys are up too. This sort of clever work and reporting!
Keep up the awesome works guys I’ve included you guys to blogroll.
8 Tips To Increase Your How Long Does Gas Safety Certificate Last Game how long does a gas safety certificate Last
The Lesser-Known Benefits Of Asbestos Cancer Lawsuit Lawyer Mesothelioma Mesothelioma Attorneys
The Reason Why You’re Not Succeeding At Hire Auto
Accident Lawyers lawyer Car Accidents
The Top 5 Reasons People Win In The Online Crypto Casino Industry Best Online Crypto Casino (Eric1819.Com)
Guide To Accident Injury Attorney: The Intermediate Guide Towards Accident Injury Attorney
Accident injury attorney [cameradb.review]
Need Inspiration? Look Up Trucking Lawyers Semi Truck Accident Lawyer Near Me
Why Do So Many People Want To Know About Best Accident Injury Lawyers?
lawyer Near me accident
Gas Safety Certificate Landlord Tools To Streamline Your Daily Life Gas Safety Certificate Landlord Trick Every Person Should Learn gas safety certificate Landlord
The Biggest Issue With Loft Bed For Sale, And How You Can Fix It
loft bed with futon
I like the valuable information you supply in your articles.
I will bookmark your weblog and test again right here regularly.
I am reasonably certain I’ll be told many new
stuff right here! Good luck for the following!
My brother suggested I may like this web site. He was once totally
right. This submit truly made my day. You cann’t consider just how so much time
I had spent for this information! Thanks!
Hello, of course this post is in fact fastidious and I have learned lot of things
from it about blogging. thanks.
My brother recommended I would possibly like this blog.
He was once totally right. This submit actually made my day.
You can not consider simply how a lot time I had spent for this information! Thank you!
The Reasons Oakland Accident Lawyer Will Be Everyone’s Desire In 2023 Accident And injury
12 Companies Leading The Way In Pragmatic Product Authentication 프라그마틱 슬롯 사이트
top togel service
Join Altogel fоr Top Toto
and Togwl Slot Gaming
Temukan permainan toto slot Ԁan togel slot paling menarik ɗі Altogel,
situs toto terpercazya untuk pengalaman bermain yang
maksimal.
10 Startups That Will Change The Capsule Coffee Maker Industry For The Better
capsule Coffee machines
A mesothelioma lawyer who has experience can help you decide the best asbestos
Litigation – pencilcause88.bravejournal.net, claim to file.
Many victims were exposed asbestos in a variety of states,
so national firms are able to file lawsuits when needed.
You’ll Never Be Able To Figure Out This Best Accident Lawyer Near Me’s Tricks best Accident lawyer near me
What’s Holding Back The Best Auto Accident Lawyers Industry?
car crash attorneys near me (Celinda)
What’s The Good And Bad About Asbestos Cancer Law Lawyer
Mesothelioma Settlement mesothelioma lawyer – Amie –
10 Misleading Answers To Common Car Accident Attorney Near Me Questions Do
You Know Which Ones? car Accident lawyer no injury
Auto Accidents Lawyer Near Me Tools To Streamline Your Everyday Life accident Car attorney
20 Reasons Why Mesothelioma Law Will Not Be Forgotten Mesothelioma compensation
10 Things You’ve Learned From Kindergarden That’ll Help You With Crypto Casino online Crypto Casino
What Experts In The Field Of Address Collection Want
You To Know? 링크모음사이트
Five Killer Quora Answers To Best Capsule Coffee Machine best capsule coffee
machine – Evangeline,
20 Trailblazers Lead The Way In Trucking Accident Lawyer Truck Accident Attorneynear Me
3 Ways That The Mesothelioma Asbestos Claim Can Influence Your
Life Mesothelioma Lawyers
A Step-By-Step Guide To Asbestos Cancer Law Lawyer Mesothelioma Settlement From Start To Finish
mesothelioma attorneys
What’s The Current Job Market For All Crypto Casinos Professionals?
All Crypto Casinos
Pragmatic Free Game: The Ugly Truth About Pragmatic Free Game
프라그마틱 무료게임 (Emery)
Reclining Chesterfield Sofa Tools To Help You Manage Your Everyday Lifethe Only Reclining Chesterfield
Sofa Trick That Everyone Should Be Able To reclining chesterfield sofa
The Most Sour Advice We’ve Ever Heard About Hiring
Auto Accident Attorneys top rated car accident lawyers (mem168new.Com)
What’s The Current Job Market For Accident & Injury Lawyers
Professionals? Accident & Injury Lawyers
15 Shocking Facts About Pragmatic Slots Free Trial 프라그마틱 환수율
10 Mobile Apps That Are The Best For Best Folding Treadmill Small Space best folding treadmill for small space
15 Latest Trends And Trends In Truck Accident Attorney truck Driver lawyer
The 10 Most Terrifying Things About Lightest 3 Wheel Rollator
Lightest 3 wheel rollator
The Comprehensive Guide To Best Crypto Online Casinos Bitcoincasinos
15 Crypto Casino Online Benefits Everybody Should Be Able To bitcoin casino
(Jacqueline)
Cryptoslots Casino Tips To Relax Your Daily Lifethe One Cryptoslots Casino Trick That Should
Be Used By Everyone Be Able To Cryptoslots casino
The 10 Most Terrifying Things About Car Replacement Key Near Me Car replacement key Near me
9 Lessons Your Parents Teach You About Recliner Couches
For Sale Recliner couches For sale
Take A Look At Your Fellow Asbestos Mesothelioma Enthusiasts.
Steve Jobs Of The Asbestos Mesothelioma Industry Mesothelioma Lawyers – Anotepad.Com,
The 10 Scariest Things About Corgi Gas Registered Engineer corgi Gas registered engineer
15 Terms Everybody Within The Link Collection Site
Industry Should Know 링크모음
A mesothelioma lawyer assists victims to file different
types claims in order to receive compensation. Personal injury and
wrongful death lawsuits are included.
My site :: asbestos case (telegra.ph)
cliquez pour lire
My coder is trying to convince me to move to .net from PHP.
I have always disliked the idea because of the expenses.
But he’s tryiong none the less. I’ve been using WordPress
on several websites for about a year and am nervous about
switching to another platform. I have heard great things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any help would be greatly appreciated!
You’ll Be Unable To Guess Sofa Couch For Sale’s Tricks sofa Couch for Sale
15 Best Saab Key Replacement Cost Bloggers You Need To Follow Saab 9-3 Key
A Step-By-Step Guide To Treehouse Bunk Bed With Slide Treehouse bed uk
It’s A Pods Coffee Machine Success Story You’ll Never Remember coffee
Pod Machine, serrano-hull-2.hubstack.net,
Great article.
10 Things That Your Family Taught You About Sectional Sofas For Sale Sectional Sofas For Sale
Why Drive Autofold Mobility Scooter Is Fast Becoming The Trendiest Thing Of 2023
auto folding mobility Scooter With suspension
How King Cock Squirting Dildo Altered My Life For The Better Squirt Dildo
5 Killer Quora Answers On Accidents Attorney Near Me Accidents Attorney Near Me
The Ultimate Glossary Of Terms About Electric Wheelchairs Near
Me electric wheelchair chair – Bill,
The Guide To Double Pushchair Sale In 2023 twin pushchair
10 Amazing Graphics About U Shaped Sectional With Chaise U Shaped Sectional Coffee Table
5 Killer Quora Answers On Wood And White Cot Bed Wood And White Cot Bed
7 Simple Tricks To Totally You Into Address Collection 주소모음사이트 (jusojula64494.blogsvila.com)
The 12 Worst Types Of People You Follow On Twitter Best Cot For Newborn
You’ll Be Unable To Guess Coffee Machine Nespresso’s Tricks coffee machine nespresso
9 Lessons Your Parents Taught You About Cribs Beds cribs beds
20 Trailblazers Leading The Way In Mid Sleeper Treehouse
Bed Bunk Bed Treehouse
30 Inspirational Quotes About Asbestos Lawsuit Payouts Asbestos Lawyers
Good day! This post could not be written any better!
Reading through this post reminds me of my good old room mate!
He always kept talking about this. I will forward this write-up to
him. Pretty sure he will have a good read. Thanks for sharing!
Hi there, I read your blogs regularly. Your writing style is awesome, keep it up!
We are a gaggle of volunteers and starting a brand new scheme in our community.
Your web site offered us with valuable info to work on. You
have performed a formidable process and our whole community will probably be thankful to you.
Hi! I know this is kind of off topic but I was wondering which blog platform
are you using for this website? I’m getting tired of WordPress because I’ve had issues with hackers and I’m looking at
options for another platform. I would be awesome if you could point me in the direction of a good platform.
I’m really enjoying the theme/design of your site. Do you ever run into any
browser compatibility problems? A number of my blog audience
have complained about my blog not operating correctly
in Explorer but looks great in Chrome. Do you have any solutions to help
fix this problem?
Ahaa, its good conversation about this paragraph here at this blog, I have read all that, so
at this time me also commenting at this place.
Hi to all, the contents existing at this web page are
actually remarkable for people knowledge, well, keep up the good work fellows.
Why You Should Concentrate On Improving Get Diagnosed With ADHD Adult Diagnosis Adhd
(Psychiatry29505.Blog-Ezine.Com)
Heya! I understand this is somewhat off-topic however I had to ask.
Does building a well-established website such as yours require
a lot of work? I am brand new to writing a blog but I do write
in my journal every day. I’d like to start a blog so I will be able to share my
experience and views online. Please let me know if you have any recommendations or tips for new aspiring
bloggers. Appreciate it!
Oh my goodness! Amazing article dude! Many thanks, However I am encountering issues with your RSS.
I don’t understand the reason why I am unable to subscribe to it.
Is there anybody getting the same RSS problems? Anyone that
knows the solution can you kindly respond? Thanx!!
I think that everything said was very logical. However, what about this?
suppose you composed a catchier post title? I ain’t
saying your content isn’t solid, but suppose you added a title that grabbed folk’s attention?
I mean What Is Pulmonary Embolism – Symptoms, Treatment And Recovery Dr
Atul Kasliwal's Blog – Cardiology, Heart Doctor, Cardiac Specialist | Dr Atul Kasliwal's Blog – Cardiology, Heart Doctor, Cardiac Specialist is kinda vanilla.
You should glance at Yahoo’s front page and note how they create news headlines to get viewers to click.
You might try adding a video or a related pic or two to get readers excited about
everything’ve written. In my opinion, it would bring your posts a little livelier.
Highly descriptive post, I enjoyed that bit. Will
there be a part 2?
Link exchange is nothing else however it is only placing the other person’s website link on your page
at proper place and other person will also do similar in support of
you.
15 Up-And-Coming Mesothelioma Legal Bloggers You Need To Check Out mesothelioma Attorney (pridgen-macdonald-3.thoughtlanes.net)
Hi there it’s me, I am also visiting this web page regularly,
this website is truly nice and the visitors are in fact sharing nice thoughts.
I’ve been surfing online more than three hours today,
yet I never found any interesting article like yours.
It is pretty worth enough for me. In my opinion, if all site owners and bloggers made good content as you did, the internet will be much more useful than ever
before.
How To Explain Best Mens Sex Toys To Your Grandparents Adult sex Toys uk
Hey would you mind stating which blog platform you’re using?
I’m going to start my own blog in the near future but I’m having a hard time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems different then most blogs and I’m looking for
something completely unique. P.S My apologies for getting off-topic
but I had to ask!
WOW just what I was searching for. Came here by searching for
Consultant SEO Paris
We recommend exploring the best quotes collections: Love And Friendship Quotes From Great People
We recommend exploring the best quotes collections: Quotes from great people
Hi! Someone in my Facebook group shared this site with us
so I came to give it a look. I’m definitely loving the information. I’m bookmarking and will be tweeting this to my followers!
Superb blog and outstanding design and style.
If some one wants to be updated with latest technologies afterward he must
be pay a quick visit this web site and be up to date all the
time.
It is perfect time to make a few plans for the longer term and
it is time to be happy. I’ve read this submit and
if I may just I wish to suggest you some interesting issues or advice.
Maybe you could write next articles relating to this article.
I wish to read more things approximately it!
WOW just what I was searching for. Came here by searching
for Situs Slot Terbaru
Thank you, I’ve just been looking for information about this subject for a while and
yours is the best I’ve found out so far. However, what concerning the bottom line?
Are you certain concerning the supply?
See What Car Door Lock Repair Near Me Tricks The Celebs Are Utilizing Car door lock repair
Hello would you mind sharing which blog platform you’re using?
I’m planning to start my own blog in the near future but I’m having a hard time deciding between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most
blogs and I’m looking for something unique.
P.S Sorry for getting off-topic but I had to ask!
It Is A Fact That Integrated Combi Microwave Is The Best Thing You Can Get.
Integrated Combi Microwave Advanced technology
How Asbestos Attorneys Altered My Life For The
Better Mesothelioma Attorney
8XBET là nhà cái uy tín hàng đầu, mang đến trải nghiệm cá cược đẳng cấp với giao diện hiện đại và hàng ngàn trò chơi hấp dẫn. Từ thể thao, slot game, 8XBET đảm bảo tỷ lệ cược tốt nhất và giao dịch siêu tốc. 8xbet.fishing
15 Gifts For The Male Masturbators Lover In Your Life mens masturbator toy
The No. Question That Everyone In Male Masturbator
Should Be Able To Answer male Masturbators uk (Busanmkt.Com)
It’s awesome for me to have a web page, which is helpful in favor of
my knowledge. thanks admin
This Week’s Most Popular Stories About Car Keys Programming program
a key [Blair]
I know this if off topic but I’m looking into starting my own weblog and was wondering
what all is required to get set up? I’m assuming having a
blog like yours would cost a pretty penny? I’m not very internet
savvy so I’m not 100% sure. Any recommendations or advice would be greatly appreciated.
Kudos
What’s The Current Job Market For Male Masturbaters Professionals?
male masturbater (Betsey)
That is a really good tip especially to those fresh to the blogosphere.
Simple but very accurate information… Many thanks
for sharing this one. A must read article!
Hello to all, how is the whole thing, I think every one is getting
more from this website, and your views are fastidious for new
visitors.
Wonderful items from you, man. I have remember your stuff previous to and you’re simply too great.
I really like what you have got here, really like what you are
saying and the way by which you are saying it.
You make it enjoyable and you still care for to stay it smart.
I can’t wait to learn far more from you. This is really a tremendous site.
Appreciate this post. Will try it out.
Hiya! I know this is kinda off topic nevertheless I’d figured I’d ask.
Would you be interested in exchanging links or maybe guest writing a blog article or vice-versa?
My blog covers a lot of the same topics as yours and I believe we could greatly benefit from each other.
If you’re interested feel free to shoot me an e-mail.
I look forward to hearing from you! Excellent blog by the way!
Hey I know this is off topic but I was wondering if you knew
of any widgets I could add to my blog that automatically
tweet my newest twitter updates. I’ve been looking for a
plug-in like this for quite some time and was hoping maybe you would
have some experience with something like this. Please let me know if you run into anything.
I truly enjoy reading your blog and I look forward to your new updates.
Hi! I know this is sort of off-topic however I needed to
ask. Does building a well-established website such as yours require
a large amount of work? I am completely new to running a blog however I do write in my journal on a
daily basis. I’d like to start a blog so I can easily share my experience and views online.
Please let me know if you have any kind of ideas or
tips for brand new aspiring blog owners.
Thankyou!
Wow, this article is pleasant, my sister is analyzing such things, therefore
I am going to tell her.
Excellent blog here! Also your site loads up fast! What host are you the
use of? Can I am getting your affiliate link on your host?
I wish my website loaded up as fast as yours lol
Your style is so unique in comparison to other people I’ve read
stuff from. Thanks for posting when you’ve got the opportunity, Guess I’ll
just book mark this page.
WOW just what I was looking for. Came here by searching
for viktnedgång med Rybelsus
7 Simple Strategies To Completely Rocking Your Electric Wheelchairs
Lightweight Power Chairs
Guide To Corgi Gas Engineer Near Me: The Intermediate Guide Towards Corgi Gas Engineer Near Me
corgi gas engineer near me – Alannah,
I’m not that much of a internet reader to be honest but your blogs really nice, keep it up!
I’ll go ahead and bookmark your website to come back down the road.
All the best
It’s going to be end of mine day, however before ending I am reading this impressive post to increase my know-how.
Wonderful blog! I found it while browsing on Yahoo News. Do you have any tips on how to get listed in Yahoo News?
I’ve been trying for a while but I never seem to get there!
Appreciate it
Your way of describing everything in this post is in fact
pleasant, every one be able to effortlessly be aware of it, Thanks a lot.
The 10 Scariest Things About Car Keys Cutting Near Me Keys Cutting Near Me
11 “Faux Pas” That Are Actually Acceptable To Make With Your Audi
Spare Key Audi Key copy
Keep this going please, great job!
Hello there! This is kind of off topic but I need some help from an established blog.
Is it hard to set up your own blog? I’m not very techincal
but I can figure things out pretty fast. I’m thinking about creating my own but I’m not sure where
to begin. Do you have any points or suggestions?
Many thanks
Wonderful blog! I found it while browsing on Yahoo News.
Do you have any tips on how to get listed
in Yahoo News? I’ve been trying for a while but I never seem to get there!
Cheers
The 15 Things Your Boss Would Like You To Know You Knew About Bentley Key Fob bentley car keys
Thanks in support of sharing such a good thought,
post is good, thats why i have read it completely
Great post however , I was wondering if you could write a litte
more on this topic? I’d be very grateful if you could elaborate a little bit
further. Appreciate it!
Don’t Forget Double Glazed Window Repair: 10 Reasons
Why You Don’t Have It Upvc Window Repair
15 Surprising Facts About Double Mattress Memory Foam double mattress Medium
firm (bitetheass.com)
Affordable Realistic Sex Dolls Tools To Ease Your Everyday Lifethe Only Affordable Realistic Sex Dolls Trick That Everybody Should Know affordable realistic Sex dolls
This piece of writing offers clear idea in support
of the new users of blogging, that genuinely how
to do running a blog.
How To Beat Your Boss With Gas Engineer Corgi Registered Gas Engineer Near Me
Guide To Accident Claim Lawyers: The Intermediate Guide For Accident Claim
Lawyers accident claim lawyer (articlescad.com)
What’s The Current Job Market For Mazda 6 Key Fob Professionals?
2010 Mazda 3 key fob Programming
An Intermediate Guide Towards Double Glazed Units
Near Me Double glaze windows
The Best Item Upgrader Tricks To Transform Your Life Best item upgrader (Autumn)
Crypto Casino Online Tools To Streamline
Your Daily Life Crypto Casino Online Trick That Everybody Should Know crypto casino online
See What Window Mechanism Repair Near Me Tricks The Celebs Are Using Window Mechanism Repair Near Me
14 Smart Strategies To Spend The Remaining Mesothelioma Lawyer Budget mesothelioma Law firms
Five Killer Quora Answers On Built In Oven And Microwave Combination built in oven and microwave combination (Tonja)
5 Killer Quora Answers To Replacement Key For Audi A3 replacement key for audi a3, Ashly,
9 Lessons Your Parents Teach You About Leather And Fabric 2 Seater Sofa leather
and fabric 2 seater sofa (Shay)
10 Things That Your Family Teach You About Audi Tt
Key Audi tt key
Guide To Pram And Stroller 2 In 1: The Intermediate Guide In Pram And Stroller 2 In 1 pram and stroller
2 in 1 (Kerry)
What You Can Use A Weekly Land Rover Discovery Key Replacement Project Can Change Your Life land rover key blank;
Zachery,
How To Tell If You’re Set For Link Collection Site 링크모음
5 Upvc Door Mechanism Projects For Any Budget Hinges For upvc doors
12 Companies Are Leading The Way In Asbestos Mesothelioma
Lawsuit Mesothelioma Lawsuits
Yesterday, while I was at work, my sister stole my iphone and tested to see if it can survive a 25 foot
drop, just so she can be a youtube sensation. My apple ipad is now destroyed and she has 83 views.
I know this is totally off topic but I had to share it with
someone!
20 Up-And-Comers To Watch In The Wheelchair Self
Propelled Industry wheelchairs self propelled (Ulrich)
You’ll Never Guess This Best Car Seats For Newborns’s Tricks Best
car seats for newborns (m1bar.com)
The 10 Most Scariest Things About Lightweight Automatic Folding Mobility Scooters Lightweight automatic folding
mobility scooter, Bookmarkstime.com,
Guide To Replacing Seal On Windows: The Intermediate Guide
To Replacing Seal On Windows replacing seal on windows (Joycelyn)
What’s The Job Market For Item Upgrades Professionals Like?
item upgrades (Kirsten)
A Handbook For Assessments For Adhd From Start To Finish Assessed for Adhd
Five Killer Quora Answers On Infant Cot Bed Infant cot bed
Cheap Comfy Couches It’s Not As Expensive As You Think Recliner sofas for sale (http://Www.metooo.It)
10 Life Lessons That We Can Learn From 2 In 1 Travel System 2 in 1 travel System pram (daly-lundqvist.mdwrite.net)
What Train Accident Cases Experts Want You To Be Able To construction Truck accident lawyer
The 10 Scariest Things About Free Standing Bio Ethanol Stove Free Standing Bio Ethanol Stove
5 Killer Quora Answers On Gas Cooker Engineer Near Me gas cooker engineer near me
You’ll Be Unable To Guess Ferrari Lost Key’s Benefits Ferrari Lost Key
The 10 Scariest Things About Bmw Replace Key bmw Replace key
What Is ADHD Treatment For Adults? History Of ADHD Treatment
For Adults what is adhd treatment for adults
You’ll Never Be Able To Figure Out This Top Pornstar Only
Fans’s Benefits top Pornstar Only Fans
Auto Folding Mobility Scooter With Suspension Tools
To Improve Your Daily Life Auto Folding Mobility
Scooter With Suspension Technique Every Person Needs To Know auto folding mobility scooter with suspension
How Window Glass Replacement Near Me Influenced My Life For The Better replacement glass for Window
[heavenchess49.Bravejournal.net]
How Best SEO Agency London Has Changed The History Of
Best SEO Agency London cheap seo Services london; filmecrestineonline.com,
Male Masterbator Tools To Ease Your Daily Life Male
Masterbator Technique Every Person Needs To Be Able To Male Masterbator
3 Common Reasons Why Your Best Chest Freezers Uk Isn’t Working (And
How To Fix It) Best small chest freezers for garage
10 Things You Learned In Kindergarden That
Will Help You Get Mini Cotbed Mini Cot Bed (tagoverflow.stream)
The 9 Things Your Parents Teach You About Spare Key Volkswagen Key Volkswagen
See What Bmw Key Cost Tricks The Celebs Are Utilizing bmw key cost (Shani)
Watch Out: How Auto Accident Attorney Near Me Is Taking Over And How To
Stop It attorney for car accident injury (Johnette)
What Is The Reason? Search Engine Optimization Agency Is Fast Increasing To Be The
Most Popular Trend For 2023? local Seo agency
3 Reasons 3 Reasons Why Your Emergency Car Locksmith Is Broken (And
How To Fix It) fobs
10 Inspirational Graphics About Baby Beds baby cots On sale
The 10 Most Scariest Things About Situs Toto Login Situs Toto Login (Situstoto-Slot94308.Blogscribble.Com)
Five Things Everybody Does Wrong Regarding Driving License C+E Kup prawo jazdy z kodem 95 (Chastity)
15 Up-And-Coming Leather Sofa With Chaise Bloggers You Need To Follow chaise sofa
Ten Scooter Driving License That Will Make Your Life Better
prawo jazdy a1, Alexandria,
10 Facts About Buy A Category B Driving License Without An Exam That Can Instantly Put You In An Optimistic Mood ile kosztuje prawo jazdy na skuter?
10 Quick Tips To B1 Driving License B1 Prawo Jazdy
10 Graphics Inspirational About Windows Aylesbury blown double glazing replacement
17 Reasons Why You Should Avoid Search Engine Optimisation Agency Seo Agency West London
5 Laws That Will Help With The Situs 4d Industry Togel resmi Indonesia
7 Easy Secrets To Totally Enjoying Your Spare Keys Car Key Cloning Service
Double Glazing Windows High Wycombe Tips From The Top In The Business emergency glazier High wycombe
You’ll Never Guess This Best Cots For Newborns’s Secrets best Cots for newborns
5 Motives How Long Does Gas Safety Certificate Last Is
Actually A Great Thing gas safety certificates, Monserrate,
Why You Should Focus On Improving Bunk Bed Small Single Bunk Beds Single Mattress
The 10 Scariest Things About Lexus Key Shell lexus Key shell
20 Rising Stars To Watch In The Address Collection Industry 링크모음사이트
10 Healthy Habits To Use ADHD Diagnosis diagnose adhd [Vernita]
How Much Do Attorney Injury Accident Attorney Experts Make?
Accident Lawyer
10 Quick Tips About Cabin Bed With Storage double cabin bed, Marshall,
Five Killer Quora Answers To Wall Fireplace fireplace
Biggest Crypto Casino Tips To Relax Your Daily Lifethe One Biggest Crypto
Casino Technique Every Person Needs To Know Biggest Crypto casino
[valetinowiki.racing]
15 Things You’re Not Sure Of About Incline Treadmill Foldable portable treadmill incline
What’s The Current Job Market For Gas Engineer Boiler
Professionals Like? Gas Engineer boiler
You’ll Never Be Able To Figure Out This Couches For Sale’s Benefits Couches for Sale
Could Pragmatic Be The Answer To 2024’s Resolving? 프라그마틱 홈페이지
Pragmatic Site: The Evolution Of Pragmatic Site 프라그마틱 슬롯무료
What Smart Car Key Replacement Is Your Next Big Obsession? Broken Car key
The Complete List Of Program Keys For Cars Dos And Don’ts programmer
I visited many web pages but the audio feature for audio songs existing at this website is in fact wonderful.
14 Cartoons About Volvo Key Fobs To Brighten Your Day volvo s60 key replacement [Damien]
9 Things Your Parents Taught You About Cot Sale cot sale (Nigel)
5 Killer Quora Answers On Affordable Cots Affordable Cots
5 Laws That Anyone Working In Link Collection Should
Know 주소모음
You’ll Never Guess This Private Adult ADHD Assessment’s Tricks Private Adult Adhd Assessment
You’ll Be Unable To Guess Private Diagnosis For ADHD’s Secrets Private Assessment For Adhd Cost
A Look At The Ugly Reality About Good Cribs Best Crib – Maps.Google.No,
Watch Out: How Window Glass Repairs Is Taking Over The World And What Can We Do About It
repair broken Window glass Near me (heavenarticle.Com)
10 Healthy Habits To Use New Audi Key new Audi keys
Solutions To The Problems Of Case Battles case battle win
Unquestionably consider that which you said. Your favourite justification seemed to be at the web
the simplest thing to have in mind of. I say to you, I certainly get irked while other folks think about concerns that they just do not recognise about.
You managed to hit the nail upon the top and outlined out the whole thing with no need side-effects , other people could take a signal.
Will probably be back to get more. Thank you
20 Great Tweets From All Time About Audi Key Workshop
The No. 1 Question That Anyone Working In Make Spare Car Key Needs To Know How To Answer How much for spare car key
10 Things Everyone Hates About Cribs Cribs Best Rated cribs (Oncokdc.ru)
Great blog you have here.. It’s hard to find high quality writing like yours these
days. I truly appreciate people like you! Take care!!
10 Things We All Hate About Timber Windows Cambridge window maintenance
See What Fascia And Soffit Installers Near Me Tricks The
Celebs Are Using fascia and soffit installers near me – Rickey –
Adult ADHD Assessment London Tools To Help You Manage Your Everyday Lifethe Only Adult ADHD Assessment London Trick That Everyone
Should Be Able To adult adhd assessment london
The 10 Scariest Things About 1kg Coffee Beans Uk 1kg coffee beans uk (images.Google.bi)
You’ll Be Unable To Guess Lpg Gas Engineer Near Me’s Tricks Lpg gas engineer
What NOT To Do When It Comes To The ADHD Assessment
For Adults Industry adhd assessment for adults cost
What Do You Know About New LG Fridge? Lg appliances refrigerator
See What Glass Repair Bristol Tricks The Celebs Are Using Glass Repair Bristol
The Ugly Real Truth Of Auto Lock Smith car auto locksmith near me
7 Tricks To Help Make The The Most Of Your Address Collection Site 주소모음
Private Adhd Assessment: The Good, The Bad, And The Ugly How To Get Assessed For Adhd
15 Top Twitter Accounts To Discover Adult Stores Near Me adult toys Sex
Hello colleagues, how is all, and what you desire to say on the topic of this post, in my
view its in fact remarkable in favor of me.
The Reason Behind Gas Engineer Has Become Everyone’s Obsession In 2024
emergency gas engineer
I do not know if it’s just me or if perhaps everybody else encountering issues with your
website. It seems like some of the written text within your posts are running off the
screen. Can somebody else please provide feedback and let me know
if this is happening to them too? This could be a issue with
my internet browser because I’ve had this happen previously.
Appreciate it
7 Easy Secrets To Totally Cannabis-Infused SEO Experts London search engine marketing agency london
Hey just wanted to give you a brief heads up and let you know
a few of the pictures aren’t loading properly. I’m not sure why but I think its a linking issue.
I’ve tried it in two different web browsers and both show
the same outcome.
What’s The Current Job Market For Togel Hongkong Professionals?
Togel Hongkong – Daftar-Akun-Togel-Resmi12656.Blog-Eye.Com –
The No. Question Everybody Working In Audi Key Replacement Should Be Able To Answer Audi Replacement Key Fob
Five Killer Quora Answers To Gas Engineers Near Me Gas engineers near me [Bill]
A Guide To Scooter Driving License In 2024 ile kosztuje Prawo jazdy na skuter (funsilo.date)
17 Signs You Work With Vauxhall Astra Replacement Key vauxhall
replacement key cost [daugaard-lang-3.mdwrite.net]
I do not even know how I ended up here, but I thought this post was great.
I don’t know who you are but certainly you’re going to a famous blogger if you are not already
😉 Cheers!
10 Websites To Help You Learn To Be An Expert In Audi Replacement Key audi Keyfob (willysforsale.Com)
See What Cots And Tots Tricks The Celebs Are Making Use Of cots
and tots (Zac)
Don’t Buy Into These “Trends” Concerning Buy A Driving License
With Code 95 ile kosztuje prawo jazdy Na skuter?
What Do You Know About Upvc Door? upvc door panels replacements
See What Gas Fire Service Engineers Near Me Tricks The Celebs Are Using gas fire service engineers
near me – Jonnie –
9 Lessons Your Parents Teach You About Wooden Cot With Bed Price wooden cot with bed price (Stan)
What The Heck What Is Sectional Sofa Bed? sectionals that Turn into beds
The Three Greatest Moments In Patio Door Locks Replacement History replacing door Locks
Five Killer Quora Answers On Wooden Sleigh Cot Bed Wooden sleigh cot bed
10 Quick Tips About 3 Wheeler Buggy top 3 wheel strollers (Doris)
The Underrated Companies To Watch In Couch Industry Curved Couches For Sale
This Is How Portable Electric Wheelchair Will
Look In 10 Years Time lightweight power Chairs
10 Facts About Treehouse Beds That Will Instantly Put You In A Good Mood play area bunk beds
15 Pragmatic Return Rate Benefits That Everyone
Should Know 프라그마틱 무료게임
10 Misconceptions That Your Boss May Have Regarding Buy A Category B Driving License Without An Exam Kup Prawo Jazdy A A1 A2 bez testu (Shad)
Beware Of This Common Mistake On Your Hob And Oven Ovens and hobs Uk
SEO Marketing London Tools To Ease Your Daily
Lifethe One SEO Marketing London Trick That Everybody Should Know
seo marketing London
Can You Ride A Mobility Scooter On The Pavement Tools To Help You Manage Your
Daily Lifethe One Can You Ride A Mobility Scooter On The Pavement Trick That Everyone Should Be Able To can You ride A Mobility scooter on the pavement
The 10 Most Scariest Things About Tread Mills Tread mills
14 Cartoons About Crypto Casino Us Which Will Brighten Your Day Crypto casino USA
5 Killer Quora Answers To Tilt And Turn Double Glazed Windows tilt and turn double glazed Windows
See What Integrated Combination Microwave Tricks The Celebs Are Using integrated combination microwave
A Trip Back In Time How People Discussed Crypto Casino
20 Years Ago online Crypto Casino
Five Killer Quora Answers To ADHD In Adult Women Treatment adhd in adult women treatment (Jeramy)
30 Inspirational Quotes On ADHD Private Diagnosis London Private Adhd Assessment Colchester
The Best Way To Explain Window Handles To Your Mom window handles for wooden frames
10 Methods To Build Your Link Collection Empire 주소모음
What’s up, every time i used to check webpage posts here in the early hours in the morning, for the reason that i
enjoy to learn more and more.
See What Mesothelioma Claim Tricks The Celebs Are Making Use Of mesothelioma (hubbard-Bitsch-2.technetbloggers.de)
Wooden Cot Single Bed Tools To Streamline
Your Everyday Lifethe Only Wooden Cot Single
Bed Trick That Everybody Should Know wooden cot single bed (Estella)
Solutions To Problems With Sofa Couch For Sale Big Couch
What A Weekly Lightweight Folding Travel Wheelchair Project Can Change Your Life folding transport wheelchair (Consuelo)
24 Hours To Improving Auto Injury Attorneys top car accident lawyers (voprosi-otveti.ru)
Large Free Standing Electric Fireplace: 11 Thing You’re Forgetting To Do free standing plug in Electric fires
You’ll Never Guess This Electric Fire For Media Wall’s Tricks
Fire For Media Wall
See What Single Push Chair Tricks The Celebs Are Using single push chair (Janessa)
5 Key Programming Myths You Should Avoid key programmer near me
A Glimpse In The Secrets Of Saab 9-3 Replacement Key Saab 9-3 Key Not Accepted Contact Service
Item Upgrader Tools To Streamline Your Daily Lifethe One
Item Upgrader Technique Every Person Needs To Learn item upgrade (Maps.Google.com.sa)
Hi there, I discovered your website by the use of Google whilst searching for a comparable
matter, your website got here up, it seems great.
I have bookmarked it in my google bookmarks.
Hi there, simply was alert to your weblog via Google, and found that it is truly
informative. I am gonna be careful for brussels. I’ll appreciate in the event you continue
this in future. Lots of other folks will probably be benefited
out of your writing. Cheers!
This Is The Complete Listing Of Best Childrens Bunk Beds Dos And Don’ts Best Bunk
See What Best Places To Buy Bunk Beds Tricks The Celebs Are Making Use Of best places to
buy bunk beds (Shirleen)
How Scooter Driving License Became The Top Trend In Social Media Kup Prawo Jazdy Kategorii B Bez Egzaminu
Chao mung ban den voi link vào bong88 nen tang ca cuoc truc tuyen hang dau danh cho nhung nguoi dam me the thao va giai tri. Website: https://bong88.wtf
hi!,I really like your writing very so much! share we keep in touch extra about your
post on AOL? I need an expert in this house to resolve my problem.
May be that is you! Looking ahead to peer you.
The Reason Behind Buy A Driving License A A1 A2 Without A Test Has Become Everyone’s Obsession In 2024 prawo jazdy A1
Why You Should Be Working On This Renault Card Key Replacement new key for
renault clio (Shenna)
Who Is Responsible For An Driving License C+E Budget? 12 Ways To Spend Your Money Kup Prawo Jazdy A A1
A2 bez testu – Reagan,
Why You Should Concentrate On Enhancing Driving License C+E Kup Prawo Jazdy A A1 A2 bez testu
A Time-Travelling Journey: How People Talked About Affordable SEO Services 20 Years Ago affordable search engine optimization Service Uk (http://www.metooo.com)
Fabulous, what a website it is! This web site gives valuable facts to us, keep it
up.
Highly energetic article, I loved that a lot.
Will there be a part 2?
The Little Known Benefits Of Buy A Driving License A A1 A2 Without A Test Ile Kosztuje Prawo Jazdy Na Skuter?
Hi there, its pleasant post concerning media print, we all be familiar with media is a fantastic source of information.
Go789 la thuong hieu ca cuoc onl duoc thanh lap tu nam 2009, nhan giay cap phep hoat dong kinh doanh hop phap tu to chuc PAGCOR. Sau nhieu nam di ra mat tren thi truong, san choi nay hien da co mat hau het tai quoc gia trong khu vuc chau A. go789s.com
Hi would you mind letting me know which hosting company you’re using?
I’ve loaded your blog in 3 completely different internet browsers and
I must say this blog loads a lot faster then most. Can you recommend a good web hosting provider at a reasonable price?
Cheers, I appreciate it!
Do you mind if I quote a few of your posts as long as I provide credit and sources back to your site?
My website is in the exact same niche as yours and my visitors would truly benefit
from a lot of the information you provide here. Please let
me know if this okay with you. Appreciate it!
I am really grateful to the owner of this web site who has shared this enormous piece of writing
at at this place.
15 Startling Facts About Driving License C+E That
You Never Knew Prawo Jazdy C+E
A Positive Rant Concerning How Much Does A Scooter Driving License Cost Prawo jazdy kat c
14 Common Misconceptions About Buy A Category B Driving License
Without An Exam ile Kosztuje Prawo jazdy na skuter
EE88 la nha cai ca cuoc truc tuyen uy tin hang dau chau A dang khang dinh vi the voi hon 12 nam hoat dong ke tu nam 2012. Duoc cap phep boi to chuc PAGCOR va so huu cong nghe bao mat tien tien tu GEOTRUST. ee88vnn.com
Hi there, its good article about media print, we all understand media is a great
source of data.
20 Trailblazers Lead The Way In How Much Does A Scooter
Driving License Cost Prawo jazdy c+e
How To Explain How Much Does A Scooter Driving License Cost
To Your Grandparents Prawo Jazdy Na Skuter
Thanks for the good writeup. It actually used to be a enjoyment account it.
Glance advanced to more introduced agreeable from you!
However, how can we keep up a correspondence?
XO88 – Nha cai top 4 hoang toc nuoc Anh ve do uy tin trong ca cuoc bong da va nhieu mon the thao khac. xo88s.win
Buy Category B Licence Online Tools To Ease
Your Daily Lifethe One Buy Category B Licence Online
Trick That Everyone Should Be Able To buy category b licence online
My spouse and I stumbled over here from a different web page and thought I should check things out.
I like what I see so i am just following you. Look forward to finding out about your
web page again.
Thank you for another great article. Where else could anyone get that
type of information in such an ideal manner of writing?
I have a presentation subsequent week, and I am at the look for such information.
15 Interesting Hobbies That Will Make You More Successful At Driving License Category C prawo Jazdy kat c
magnificent issues altogether, you just gained a logo new reader.
What might you recommend about your publish that you made a few days in the past?
Any sure?
Undeniably believe that which you said. Your favorite reason appeared to
be on the internet the simplest thing to be aware
of. I say to you, I certainly get irked while people think about worries that they plainly don’t know about.
You managed to hit the nail upon the top and also defined out the whole thing without having side-effects , people could take a signal.
Will probably be back to get more. Thanks
It’s amazing to pay a quick visit this web page and reading the views of all
colleagues on the topic of this article, while I am also eager of
getting familiarity.
Yes! Finally something about Dedy permadi.
I think this is one of the most vital information for me. And i’m glad reading your article.
But should remark on few general things, The web site style is great, the articles is
really excellent : D. Good job, cheers
I was able to find good information from your blog articles.
I like reading a post that can make men and women think.
Also, many thanks for allowing for me to comment!
The Most Effective Reasons For People To Succeed On The How Much Does
A Scooter Driving License Cost Industry prawo jazdy c+e (Etsuko)
Its like you read my mind! You appear to know
so much about this, like you wrote the book in it or something.
I think that you can do with a few pics to drive the message home a little bit, but
instead of that, this is fantastic blog. A great read.
I’ll definitely be back.
The Ultimate Guide To Buy A Driving License A A1 A2 Without A Test b1
prawo jazdy – Patsy,
I was wondering if you ever thought of changing the structure of your
website? Its very well written; I love what youve
got to say. But maybe you could a little more in the way of content so
people could connect with it better. Youve got an awful lot of text for only having 1 or 2 pictures.
Maybe you could space it out better?
Hello! I know this is kinda off topic but I
was wondering if you knew where I could locate a captcha
plugin for my comment form? I’m using the same blog platform as yours and I’m
having problems finding one? Thanks a lot!
wonderful put up, very informative. I ponder why the other experts of this sector do not realize this.
You must proceed your writing. I’m sure, you have a huge readers’ base
already!
15 Best Documentaries About Scooter Driving License prawo jazdy kat c
Driving License Category C Explained In Fewer Than 140 Characters ile kosztuje prawo jazdy na skuter?
78win la nen tang ca cuoc truc tuyen hang dau Dong Nam A. Nha cai thu hut hon 1 trieu nguoi choi moi ngay. 78win khong ngung doi moi de mang lai trai nghiem tot nhat. 78win dan dau ve cong nghe bao mat khach hang. Uu dai hap dan nhu thuong nap 100% thu hut dong dao nguoi choi. 78winvna.com
Link exchange is nothing else except it is just placing the other person’s webpage link on your page at appropriate place and other person will also do similar for you.
Very good blog! Do you have any suggestions for aspiring writers?
I’m hoping to start my own blog soon but I’m a little lost on everything.
Would you advise starting with a free platform like WordPress or go for
a paid option? There are so many choices out there that I’m totally overwhelmed ..
Any ideas? Bless you!
Thanks on your marvelous posting! I genuinely enjoyed
reading it, you could be a great author. I will be sure to bookmark your blog and definitely will
come back very soon. I want to encourage continue your great
job, have a nice day!
If you’re a fan of action-packed fruit-slicing games, Slice Master is a title you don’t want to miss. Slicemaster.net
I’ll immediately grab your rss as I can’t find your email subscription hyperlink or newsletter service.
Do you have any? Please permit me understand in order that I could subscribe.
Thanks.
This is very interesting, You’re a very skilled blogger. I have joined your rss feed and look forward to seeking more of your great post.
Also, I have shared your website in my social networks!
I read this piece of writing completely on the topic of the difference of latest and preceding technologies,
it’s amazing article.
Chao mung ban den voi 8XBET – diem den hang dau danh cho nhung ai dam me ca cuoc va giai tri truc tuyen! shidefc.com
Do you have any video of that? I’d want to find out more details.
Excellent way of telling, and pleasant post to get information concerning my presentation topic, which i am going to deliver
in university.
77bet la cong game truc tuyen lon nhat tai Viet Nam hien nay. Tai 77bet, ban co the tham gia choi game bai doi thuong get.lgbt
I was wondering if you ever considered changing the structure of your site?
Its very well written; I love what youve got to say. But maybe you could a little more
in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
What’s up to every body, it’s my first visit of this blog; this webpage
contains awesome and actually good stuff for
readers.
Thanks for any other wonderful post. Where else may anybody get that kind of information in such an ideal approach of
writing? I’ve a presentation next week, and I’m on the look for such information.
Wow, this post is pleasant, my younger sister is analyzing these kinds of things, thus I am going to let know her.
Qh88 is an online gambling house that ensures prestige and is trusted and chosen by many customers. The bookmaker is licensed to operate legally and is issued by Internet Gaming Licensees (IGL). QH88 meets the criteria: prestige, transparency, safety, giving players a top-notch betting experience. https://lacquerous.com/
V9BET la nha cai truc tuyen cung cap da dang cac san pham giai tri va co he thong bao mat hien dai, dich vu cham soc khach hang chuyen nghiep. discovermccall.com
Lux39 la cong game bai doi thuong uy tin nhat Dong Nam A, cac tua game doi thuong hap dan: Baccarat, Mau binh doi thuong… lux39.net
Если вам нужен качественный ремонт, порекомендуем: Ремонт телевизоров Philips
J88 là cổng game đổi thưởng và cá cược trực tuyến hàng đầu, nơi hội tụ đầy đủ các sản phẩm giải trí hấp dẫn như thể thao, nổ hũ, bắn cá và hơn thế nữa. rarerooms.io
qh88 la mot nen tang ca cuoc truc tuyen uy tin, chuyen cung cap cac dich vu ca cuoc the thao, game bai, va xo so. qh88.wang
I am extremely impressed with your writing skills and also with
the layout on your blog. Is this a paid theme or did you modify it yourself?
Either way keep up the excellent quality writing, it’s rare to see a nice blog like this one nowadays.
This is a really good tip especially to those fresh to
the blogosphere. Brief but very precise info… Many thanks for sharing this one.
A must read article!
Verry nice article, totgally what I wanted to find. https://www.waste-ndc.pro/community/profile/tressa79906983/
This design is wicked! You definitely know how to keep a
reader entertained. Between your wit and your videos, I was almost moved to
start my own blog (well, almost…HaHa!) Wonderful job.
I really enjoyed what you had to say, and more than that, how you presented it.
Too cool!
If you are a fan of adventure and racing games, you’ve probably heard of Run3.biz — one of the most popular 3D running games out there
I got this web page from my buddy who shared with me concerning this web page and
at the moment this time I am browsing this site and reading very informative articles at this time.
Fantastic beat ! I would like to apprentice whilst you amend your web site, how
can i subscribe for a blog web site? The account aided me
a acceptable deal. I had been a little bit familiar of this your broadcast
provided vivid transparent concept
king88 itsthedubliners la nha cai truc tuyen hang dau tai Viet Nam, KING88 cung cap da dang tro choi hap dan tu ca cuoc the thao, baccarat, blackjack den slot machine. itsthedubliners.com
Excellent way of explaining, and good paragraph to get facts on the topic
of my presentation focus, which i am going to convey in university.
Hello, I read your blog daily. Your story-telling style is awesome, keep
it up!
Admiring the time and effort you put into your site and in depth information you present.
It’s awesome to come across a blog every once in a while that isn’t the same unwanted rehashed material.
Wonderful read! I’ve saved your site and I’m adding your RSS feeds to my Google account.
What’s Happening i’m new to this, I stumbled upon this I have found It positively useful and
it has aided me out loads. I am hoping to give a contribution & assist different
customers like its helped me. Great job.
Fun88 la nha cai ca cuoc truc tuyen hoat dong duoi su quan ly cua tap doan OG Global Access Limited va duoc cap phep boi PAGCOR Philippines cung Isle of Man Gaming Authority. fun88.surf
After exploring a handful of the articles on your
blog, I seriously appreciate your technique of blogging.
I book-marked it to my bookmark webpage list and
will be checking back soon. Please check out my website as well and tell me
what you think.
It’s amazing to go to see this web site and reading the
views of all friends on the topic of this piece of writing, while I
am also keen of getting familiarity.
Hmm it appears like your site ate my first comment (it was extremely long) so I guess I’ll just sum it up what I submitted and say, I’m thoroughly enjoying your blog.
I too am an aspiring blog writer but I’m still new to everything.
Do you have any suggestions for rookie blog writers?
I’d really appreciate it.
At this moment I am ready to do my breakfast, when having my breakfast coming over again to read other news.
Pretty section of content. I just stumbled upon your blog and in accession capital
to assert that I acquire actually enjoyed account your
blog posts. Anyway I’ll be subscribing to your feeds and even I achievement you access consistently
fast.
Good day! I could have sworn I’ve been to this website before but after checking
through some of the post I realized it’s new to me.
Nonetheless, I’m definitely glad I found it and I’ll be
book-marking and checking back frequently!
Excellent blog you have here.. It’s hard to find high-quality writing like yours nowadays.
I seriously appreciate people like you! Take care!!
I was suggested this blog by my cousin. I’m not sure whether this post is written by him
as no one else know such detailed about my problem.
You’re incredible! Thanks!
hey there and thank you for your information – I
have definitely picked up something new from right here.
I did however expertise several technical issues using this site, as I experienced to reload the site many times
previous to I could get it to load correctly. I had been wondering if your hosting is OK?
Not that I am complaining, but slow loading instances times will
very frequently affect your placement in google and
could damage your high-quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my e-mail and can look out for a
lot more of your respective fascinating content.
Make sure you update this again soon.
With havin so much content do you ever run into any issues of plagorism or copyright infringement?
My website has a lot of completely unique content I’ve either authored myself or outsourced but
it seems a lot of it is popping it up all over the internet without my permission. Do you know any
methods to help prevent content from being ripped off?
I’d certainly appreciate it.
Hello there! Do you know if they make any plugins to
help with SEO? I’m trying to get my blog to rank for some targeted keywords but
I’m not seeing very good gains. If you know of any please share.
Thanks!
I think the admin of this web page is genuinely working hard for his website, as here every data is
quality based data.
Vn88 duoc gioi chuyen gia cung nhu cac cuoc thu danh gia la mot thuong hieu doi thuong uy tin hien nay. Tai day so huu nhieu tro choi da dang va hap dan bac nhat thi truong. vn88.company
I was pretty pleased to find this web site. I need to to thank you for
your time for this particularly wonderful read!! I definitely
liked every part of it and I have you book marked to look at new information in your website.
Wow, superb blog layout! How long have you been blogging for?
you make blogging look easy. The overall look of your
web site is excellent, as well as the content!
789club la cong game doi thuong so 1 Viet Nam hien nay, noi tieng voi cong dong nguoi choi len toi hang trieu nguoi choi. 789club.menu
Asking questions are genuinely pleasant thing if you are
not understanding something entirely, but this article offers fastidious understanding even.
Incredible points. Sound arguments. Keep up the good
effort.
I could not resist commenting. Perfectly written!
Aw, this was an exceptionally nice post. Finding
the time and actual effort to create a good article…
but what can I say… I procrastinate a whole lot and never seem to get nearly anything done.
Excellent goods from you, man. I have be aware your stuff prior to and
you are simply extremely fantastic. I really like what
you have received here, certainly like what you are saying and
the way through which you assert it. You are making it entertaining and
you continue to care for to keep it sensible.
I can not wait to read much more from you. This is really a wonderful
site.
Hi there, yeah this piece of writing is truly good
and I have learned lot of things from it concerning blogging.
thanks.
This page definitely has all of the information I wanted about this subject
and didn’t know who to ask.
Go88 la cong game doi thuong truc tuyen so 1 Viet Nam hien nay voi hon 2 trieu nguoi choi moi ngay tai trang chu Go88 COM. duojs.org
fantastic submit, very informative. I’m wondering why the other specialists of
this sector don’t understand this. You should continue your writing.
I am confident, you’ve a great readers’ base
already!
Nice post. I learn something totally new and challenging on sites I stumbleupon every day.
It’s always helpful to read through content from other authors and practice a little something from
other websites.
I got this website from my pal who told me concerning this
web page and now this time I am visiting this web
page and reading very informative posts at this place.
Anh em nen som dung chan o Nhà cái VN88 de co nhieu trai nghiem muot ma nhu y hon nua. San choi cong bang, minh bach, nhan van ke tren co 13 nam kinh nghiem. vn88tk2.com
V9BET – nha cai ca cuoc quoc te voi tru so chinh tai Manila, Philippines phuc vu hon 6.300 luot dang ky moi ngay tai thi truong Viet Nam. Duoc cap phep boi First Cagayan va CEZA. v9betnet.com
iwin – Noi quy tu dang cap cua gioi thuong luu, la mot trong nhung cong game bai doi thuong uy tin nhat hien nay tai thi truong Chau A. cffresearch.org
An interesting discussion is definitely worth comment.
I think that you need to publish more on this subject matter,
it may not be a taboo subject but generally folks don’t discuss such issues.
To the next! Cheers!!
Hello there! I know this is kind of off topic but I was wondering which blog platform are you using for this site?
I’m getting fed up of WordPress because I’ve had issues with hackers
and I’m looking at alternatives for another platform.
I would be fantastic if you could point me in the direction of a good platform.
“SV388 la mot trong nhung nen tang ca cuoc da ga truc tuyen uy tin hang dau tai chau A, mang den trai nghiem chan thuc va hap dan cho nguoi yeu thich bo mon nay. Voi he thong truyen hinh truc tiep chat luong cao . sv388-games.com
“
information.|My family members every time say that I am killing my time here
pokračujte v pěkné práci, kolegové.|Když máte tolik obsahu a článků, děláte to?
devido a esta maravilhosa leitura!!! O que é que eu acho?
A person necessarily lend a hand to make critically articles I’d state.
That is the first time I frequented your website page
and so far? I surprised with the analysis you made to make this actual
post amazing. Great task!
at web, except I know I am getting familiarity all the time by reading thes pleasant posts.|Fantastic post. I will also be handling some of these problems.|Hello, I think this is a great blog. I happened onto it;) I have bookmarked it and will check it out again. The best way to change is via wealth and independence. May you prosper and never stop mentoring others.|I was overjoyed to find this website. I must express my gratitude for your time because this was an amazing read! I thoroughly enjoyed reading it, and I’ve bookmarked your blog so I can check out fresh content in the future.|Hi there! If I shared your blog with my Facebook group, would that be okay? I believe there are a lot of people who would truly value your article.|منشور رائع. سأتعامل مع بعض هذه|
My brother suggested I would possibly like this blog.
He was totally right. This publish truly made my day. You cann’t believe simply how so much time I
had spent for this information! Thank you!
Good day very nice site!! Man .. Excellent ..
Wonderful .. I will bookmark your web site and take the feeds also?
I’m glad to find numerous helpful information right here in the put up, we
want develop more techniques in this regard, thanks for sharing.
. . . . .
Looking for an exciting game that challenges your skills, keeps you engaged, and helps you unwind? Run 3 is the perfect choice for anyone who loves endless running games but wants a unique twist. run3.bio
What’s up to all, how is all, I think every one is getting more from this
site, and your views are fastidious in favor of
new viewers.
Fiquei muito feliz em descobrir este site. Preciso de agradecer pelo vosso tempo
Hey there! Would you mind if I share your blog with my twitter
group? There’s a lot of folks that I think would really appreciate your content.
Please let me know. Thanks
Hi there it’s me, I am also visiting this web site daily, this web page is actually pleasant
and the people are actually sharing nice thoughts.
Kubet88 – Link vao trang chu KU BET moi nhat 2024. KUBET88 chuan dang co khuyen mai 88k danh cho hoi vien moi, tham gia ngay hom nay. markusklinko-indrani.com
Roy79 is licensed to operate legally by Isle of Man Gambling. This is Asia’s leading reputable online betting address. Download the Roy79 app now to play card games for prizes! https://roy79.vip/
I was curious if you ever thought of changing the structure of your blog?
Its very well written; I love what youve got to say. But maybe you could a little
more in the way of content so people could connect with it better.
Youve got an awful lot of text for only having one or 2 images.
Maybe you could space it out better?
nogensinde løbe ind i problemer med plagorisme eller krænkelse af ophavsretten? Mit websted har en masse unikt indhold, jeg har
Sao79 Club or Sao Win is a reputable card game portal with more than 500,000 downloads by 2024. Enjoy playing card games, Sic Bo, coin toss, fish shooting, lottery… Sao79 allows cross-platform transactions via Momo Pay, scanned bank codes, transfer, Zalo Pay, scratch cards… along with quick withdrawals to bank accounts, ATM cards. https://sao79.vip/
Duoc menh danh la cong game uy tin so 1 thi truong, Red79 se khong lam anh em that vong.
Neu anh em dang san tim dia chi ca cuoc truc tuyen uy tin thi nen som dung chan tai tx79 tx79.vip
Рекомендую Взломать вибер . Проверенные хакеры, которые предоставляют профессиональные услуги.
Hi to every one, it’s in fact a good for me to pay a visit this website,
it consists of useful Information.
I used to be able to find good information from your blog posts.
Kan du anbefale andre blogs / websteder / fora, der beskæftiger sig med de samme emner?
Рекомендую https://telegra.ph/Uslugi-vzloma-kak-ya-vybral-nadezhnogo-specialista-dlya-svoih-zadach-12-15-2 . Проверенные хакеры, которые предоставляют профессиональные услуги.
That is a good tip particularly to those new to
the blogosphere. Short but very accurate
info… Thanks for sharing this one. A must read article!
I like what you guys are up too. This type of clever work and coverage!
Keep up the excellent works guys I’ve incorporated
you guys to our blogroll.
Рекомендую https://telegra.ph/Kak-ya-nashel-hakerov-dlya-vzloma-realnye-metody-i-proverennye-resursy-12-15-2 . Проверенные хакеры, которые предоставляют профессиональные услуги.
It is not my first time to pay a visit this web site, i am browsing this
web page dailly and get pleasant information from here all the time.
Nhung trai nghiem muot ma nhu y tai cong game pem789 da giup nhieu nguoi giai toa cang thang hieu qua. pem789.vip
الاستمرار في توجيه الآخرين.|Ahoj, věřím, že je to vynikající blog. Narazil jsem na něj;
If you want to take a great deal from this post then you have
to apply such strategies to your won webpage.
Loto188 mang den cho nguoi choi mot kho tang game da dang, tu cac tro choi dan gian quen thuoc den nhung tua game hien dai, dap ung moi nhu cau giai tri cua ban . loto188casino.net
I just like the valuable information you supply in your articles.
I’ll bookmark your blog and take a look at again here frequently.
I’m rather certain I will be told a lot of new stuff proper right here!
Good luck for the following!
San choi cong bang, minh bach, nhan van hang dau Chau A goi ten vic79.vip. Anh em nen som dang ky lam thanh vien de co trai nghiem muot ma nhu y.
que eu mesmo criei ou terceirizei, mas parece que
Greetings from Ohio! I’m bored at work so I decided to browse your site on my iphone during lunch break. I really like the knowledge you present here and can’t wait to take a look when I get home. I’m amazed at how quick your blog loaded on my phone .. I’m not even using WIFI, just 3G .. Anyhow, amazing site!
A person necessarily lend a hand to make seriously posts I would
state. This is the first time I frequented your website page
and thus far? I surprised with the analysis you made to
make this actual put up extraordinary. Great task!
play su789 vin la dia chi ca cuoc truc tuyen uy tin hang dau thi truong Chau A. Tai app Su789 voi giao dien dep mat cung 20300 on dinh tren da nen tang, hop voi IOS, Android la the manh cua san choi nay.. su789.app
What’s up, for all time i used to check website posts here early in the morning, since i like to
find out more and more.
Simply want to say your article is as astonishing.
The clearness in your post is simply spectacular
and i can assume you’re an expert on this subject. Well with your permission allow me to grab your RSS feed to keep updated with forthcoming post.
Thanks a million and please carry on the enjoyable work.
Very nice post. I just stumbled upon your blog and wanted to say that I have really enjoyed browsing your blog posts.
In any case I will be subscribing to your feed and I hope you
write again soon!
que eu mesmo criei ou terceirizei, mas parece que
Wow, that’s what I was seeking for, what a stuff! existing
here at this weblog, thanks admin of this website.
KUBET – kubet88 la nha cai ca cuoc online uy tin hang dau tai thi truong Viet Nam, cung cap nhieu tro choi ca cuoc hap dan nhu xo so, bong da… Kubet.buzz trang chu ho tro, dang ky, dang nhap Kubet chinh thuc.
For Sale: Database of Casino Players in Europe
Are you looking for a way to expand your customer base and increase your business revenue? We have a unique offer for you! We are selling an extensive database of casino players from Europe that will help you attract new clients and improve your marketing strategies.
What does the database include?
• Information on thousands of active casino players, including their preferences, gaming habits, and contact details.
• Data on visit frequency and betting amounts.
• The ability to segment by various criteria for more precise targeting.
The total database contains 2 million players. Data is from 2023. The database is active, and no mailings have been conducted yet.
The price for the entire database is 5000 USDT.
The price for 1 GEO is 700 USDT.
Tier 1 countries.
For any details, please contact me:
Telegram: https://t.me/Cybermoney77
Com tanto conteúdo e artigos, alguma vez se deparou com problemas de plágio ou violação de direitos de autor? O meu site tem muito conteúdo exclusivo que eu próprio criei ou
Můžete mi doporučit nějaké další blogy / webové stránky / fóra, které se zabývají stejnými tématy?
Hello to every body, it’s my first pay a quick visit of this blog; this weblog carries awesome and truly fine information in support of visitors.
Chao mung ban den voi 8XBET – nen tang ca cuoc truc tuyen hang dau tai Viet Nam! De giup ban de dang tiep can va trai nghiem nhung tro choi dinh cao. 8xbet.spa
jun88 la mot trong nhung nen tang ca cuoc truc tuyen hang dau tai Viet Nam, mang den cho nguoi choi trai nghiem giai tri dinh cao voi hang loat san pham da dang. jun88.team
7 Helpful Tips To Make The Most Out Of Your Best
SEO Program backlinks
Five Killer Quora Answers On American Fridges Freezers american fridges freezers
) Znovu ho navštívím, protože jsem si ho poznamenal. Peníze a svoboda je nejlepší způsob, jak se změnit, ať jste bohatí a
What’s The Current Job Market For Treadmill Foldable Electric Professionals?
treadmill foldable electric
Hey! Quick question that’s completely off topic. Do you know how to make your site mobile
friendly? My blog looks weird when viewing from my iphone.
I’m trying to find a template or plugin that might be able to correct this problem.
If you have any suggestions, please share. Appreciate it!
A Guide To Replace Upvc Door Panel From Beginning
To End replacement upvc door panels
10 Locations Where You Can Find Best SEO Software UK seo Traffic Software
It is actually a nice and useful piece of info.
I am happy that you simply shared this useful info with us.
Please keep us informed like this. Thank you for sharing.
188Bet
is a corporation that meets reputable bookmaker standards, currently ranked top 1 in Asia. With a variety of products from online soccer betting, online casino to top card games, 188 Bet always maintains its position against other competitors such as W88, M88, FB88…
99OK
is the most VIP online casino house in Vietnam, 99ok com offers a diverse game store from football betting, Sic Bo, lottery to interesting casino games. With a smooth interface, attractive promotions and strong security system, 99OK certainly brings you a top-notch, safe betting experience.
Nice post. I was checking continuously this blog and I’m impressed!
Extremely helpful info particularly the closing phase 🙂 I take care of such info much.
I was seeking this particular information for a very lengthy time.
Thanks and good luck.
What To Look For In The What Is SEO Software That Is Right For
You Seo Tools
Hi there I am so happy I found your weblog, I really
found you by accident, while I was browsing on Digg for something else, Nonetheless I am here now and
would just like to say kudos for a remarkable post and
a all round enjoyable blog (I also love the
theme/design), I don’t have time to look over
it all at the moment but I have saved it and also included your
RSS feeds, so when I have time I will be back to read much
more, Please do keep up the fantastic work.
Com tanto conteúdo e artigos, vocês já se depararam com algum problema de plágio?
I love your blog.. very nice colors & theme. Did you design this website yourself or
did you hire someone to do it for you? Plz respond as I’m looking
to construct my own blog and would like to find out where u got this from.
thanks a lot
SEO Optimizer Software Tools To Ease Your
Everyday Lifethe Only SEO Optimizer Software Trick Every Individual Should Know Seo Optimizer
Software (Woojincopolymer.Co.Kr)
What To Look For In The Modern Wood Burner Right For
You Modern wood Burning stove
information.|My family members every time say that I am killing my time here
Sunwin – The most prestigious Rewards Card Game Paradise. The game portal is sought after and participated by a large number of players. The prize exchange games at Hit Club are diverse: Mau Binh, Tien Len Counting Leaves, Phỏm, Sam Loc, Sic Bo, Sic Bo, Crab Bau, Fish Shooting, etc.
Lu88 has built a huge game store with more than 600 different betting genres. In addition to the main sports, the house also has online casino, fish shooting, lottery, cockfighting, lottery spinning… Lu88’s modern, professional betting platform will help players have a safe and transparent experience. transparent, attractive. Please join now at this link: https://lu888.info/
10 Misconceptions Your Boss Shares Concerning
Leather Recliners For Sale 3 seater sofa sale (Cecelia)
fb88 đăng nhập – diem den hang dau danh cho nhung nguoi dam me ca cuoc bong da uy tin va chuyen nghiep. fb88.photo
Můžete mi doporučit nějaké další blogy / webové stránky / fóra, které se zabývají stejnými tématy?
Chao mung ban den voi M88 – nen tang ca cuoc truc tuyen uy tin va chat luong hang dau tai Viet Nam! m88.ad
great publish, very informative. I wonder why the opposite experts of this sector do not realize this.
You must continue your writing. I’m sure, you’ve a great readers’ base already!
Hi, i read your blog occasionally and i own a similar one and i
was just wondering if you get a lot of spam responses?
If so how do you stop it, any plugin or anything you can suggest?
I get so much lately it’s driving me insane so any assistance is
very much appreciated.
Do Not Buy Into These “Trends” About SEO Tools software for seo (Tanja)
Hey there! This is my 1st comment here so I just wanted to give a quick shout out and tell you I
truly enjoy reading through your blog posts. Can you suggest any other blogs/websites/forums that go over the same subjects?
Many thanks!
hello there and thank you for your information –
I have definitely picked up anything new from right here.
I did however expertise a few technical points using
this site, as I experienced to reload the site lots of times previous to I could get it to load correctly.
I had been wondering if your web host is OK? Not that I’m complaining,
but slow loading instances times will often affect your placement in google and could damage your
high-quality score if advertising and marketing with Adwords.
Anyway I’m adding this RSS to my email and can look out for much
more of your respective interesting content. Make
sure you update this again soon.
link w88 la nha cai uy tin hang dau voi hang trieu nguoi choi tin tuong tren toan the gioi. Tai day, ban se tim thay link truy cap chinh thuc vao w88in.vip moi nhat
LG Frigde Tools To Streamline Your Life Everyday Lg Larder Fridge
vykřiknout a říct, že mě opravdu baví číst vaše příspěvky na blogu.
Thanks for sharing your thoughts about Roulette en Ligne.
Regards
The Advanced Guide To Test For ADHD In Adults Testing For Adhd
fun88 đăng nhập la nha cai uy tin va noi tieng hang dau tai chau A, duoc hang trieu nguoi choi tin tuong lua chon. Voi link vao chinh thuc duoc cap nhat moi nhat thang 12/2024. fun88b.co
Guide To Misty Windows Repair Near Me: The Intermediate Guide For Misty Windows Repair Near Me
misty Windows repair near me (tawassol.univ-Tebessa.Dz)
e dizer que gosto muito de ler os vossos blogues.
Эта статья предлагает живое освещение актуальной темы с множеством интересных фактов. Мы рассмотрим ключевые моменты, которые делают данную тему важной и актуальной. Подготовьтесь к насыщенному путешествию по неизвестным аспектам и узнайте больше о значимых событиях.
Изучить вопрос глубже – https://nakroklinikatest.ru/
Top-Rated Mobility Scooters Tools To Ease Your Daily Life Top-Rated Mobility Scooters Trick
That Everyone Should Know Top-rated mobility Scooters, git.gqnotes.com,
Hello, I log on to your blogs like every week. Your story-telling style
is witty, keep doing what you’re doing!
Sunwin chính thức cập nhật thêm domain chính hãng trong tháng 12/2024. Sunwin tặng code tân thủ 199k trong T12 mừng sự kiện ra mắt domain mới tại sunwin20a.com
Learn More About Subaru Car Keys While Working From Your Home Subaru Remote Key
33win la diem den ly tuong cho nhung nguoi yeu thich ca cuoc truc tuyen, cung cap da dang san pham nhu ca cuoc the thao, slot game, va nhieu tro choi hap dan khac. 33win.monster
Hey there! This is kind of off topic but I need some help from an established blog.
Is it very hard to set up your own blog? I’m not very techincal but I can figure things out pretty fast.
I’m thinking about creating my own but I’m not sure where to start.
Do you have any ideas or suggestions? Cheers
Post writing is also a fun, if you be familiar with then you
can write or else it is difficult to write.
17 Signs You Are Working With Mystery Box best mystery Boxes
MAX88 – Đẳng cấp cá cược online đến từ Anh Quốc. Thử sức với MAX88 qua các trò chơi như Tài Xỉu, Xóc đĩa và Cá cược bóng đá .
skupině? Je tu spousta lidí, o kterých si myslím, že by se opravdu
You’ll Never Guess This Cost Replacement Car Key’s Tricks Cost Replacement Car Key, http://Www.Google.Co.Mz,
Link Collection Site Tips From The Top In The Industry 주소모음사이트
After looking over a few of the articles on your web page, I seriously appreciate your technique of writing a blog.
I book marked it to my bookmark webpage list and will be checking back in the near future.
Please visit my website too and tell me your opinion.
hi88 la mot trong nhung cong game doi thuong hang dau tai Viet Nam, noi ban co the trai nghiem vo van tro choi hap dan tu ca cuoc the thao den cac tro choi truc tuyen. gaudiexhibitioncenter.com
Chao mung ban den voi kubet – nen tang giai tri uy tin va dang cap hang dau tai Viet Nam. Truy cap ngay link moi nhat de kham pha hang loat tro choi hap dan tu game bai, slot, no hu den ca cuoc the thao. kubet20.com
Guide To Accident Claim Lawyers: The Intermediate Guide On Accident Claim Lawyers accident claim lawyer
Why Truck Attorney Near Me Isn’t A Topic That People Are Interested In Truck Attorney Near Me best Semi truck Accident attorney
How Truck Accident Attorney For Hire Has Changed The History Of Truck Accident Attorney For Hire semi truck accident lawyers near me
The Top 5 Reasons People Thrive In The Truck Attorneys Near Me Industry truck accidents attorneys (Lida)
Hi would you mind stating which blog platform you’re working with?
I’m planning to start my own blog soon but I’m having a difficult time selecting between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your layout seems different then most blogs and I’m looking for something unique.
P.S Apologies for being off-topic but I had to ask!
Рекомендую – сервисный ремонт пылесосов дайсон
You’ll Be Unable To Guess Hobs Oven’s Secrets hobs
oven (Seth)
Guide To Hobs Oven: The Intermediate Guide For Hobs
Oven hobs oven – Louie,
It’s The Myths And Facts Behind Car Accidents Lawyer
Near Me car injury attorney near me
Accident Injury Lawyers Near Me Tools To Ease Your Daily Lifethe One Accident
Injury Lawyers Near Me Trick Every Person Should Know accident injury lawyers near me – Todd
–
Ten Things You Learned At Preschool To Help You Get A Handle On Robot Vacuum Cleaner Sale best robot vacuum Under 200
Definitely imagine that which you said. Your favourite reason appeared to
be on the net the simplest thing to take into account of.
I say to you, I definitely get annoyed at the same time as other folks consider worries
that they just do not understand about. You managed to
hit the nail upon the highest as smartly as defined out the entire thing with no need side effect , folks could take a signal.
Will probably be back to get more. Thanks
Back Injury Compensation Claims: The Good And Bad
About Back Injury Compensation Claims injury attorneys near me [Graciela]
5 Killer Quora Answers On Robotic Vacuum Cleaner Robotic Vacuum Cleaner Sale, Telegra.Ph,
Clubbing 압구정오피
What Do You Think? Heck What Exactly Is Asbestos Exposure Lawyer?
Asbestos lawsuit
Five Killer Quora Answers To Best Ovens Uk Ovens Uk
The Ugly Facts About Asbestos Attorney Mesothelioma mesothelioma attorneys (Jasmin)
Oven And Hob Tools To Make Your Daily Life Oven And Hob Trick Every
Person Should Know oven
Best Robot Cleaner 101:”The Ultimate Guide For Beginners Automatic Cleaning Robot
The 10 Scariest Things About 2 Seater Fabric Sofa Uk 2 seater Fabric sofa uk
See What Sectional L Shaped Sectional Tricks The Celebs Are Using sectional l shaped – Ruth,
British Wood Burning Stoves Tools To Ease
Your Daily Life British Wood Burning Stoves Trick That
Every Person Must Learn British Wood Burning Stoves
Chao mung ban den voi bong88 style – nen tang ca cuoc truc tuyen hang dau danh cho tin do the thao va giai tri. Bong 88 cam ket mang den trai nghiem ca cuoc dinh cao voi da dang loai keo va ty le canh tranh. bong88.style
fb88 tu hao la mot trong nhung nha cai truc tuyen hang dau, mang den trai nghiem giai tri da dang va chat luong. gerardmalanga.com
See What Dual Fuel Range Cookers Uk Tricks The Celebs Are Using
dual fuel range cookers uk – Shane,
Assessment For Mental Health Tips From The Most Effective In The Industry Mental Health diagnostic assessment online
Рекомендую – рейтинг скороварок из нержавеющей стали
Esta página tem definitivamente toda a informação que eu queria sobre este assunto e não sabia a quem perguntar. Este é o meu primeiro comentário aqui, então eu só queria dar um rápido
Рекомендую – скороварка какая лучше
Five Killer Quora Answers To SEO Company UK Seo company uk
This Week’s Most Popular Stories About Gas Safe Registered Engineer
Near Me Gas Safe Registered Engineer Near Me
gas safe Heating engineer
m88 unsanenyc noi mang den nhung co hoi ca cuoc truc tuyen hap dan nhat tai Viet Nam. Voi link dang ky va dang nhap M88 luon duoc cap nhat nhanh chong. unsanenyc.com
jun88 la mot trong nhung nen tang ca cuoc truc tuyen hang dau tai Viet Nam, mang den cho nguoi choi nhung trai nghiem giai tri tuyet voi voi nhieu san pham da dang.
It’s very effortless to find out any matter on net as compared to books,
as I found this article at this web page.
MAX88 – Đẳng cấp cá cược online đến từ Anh Quốc. Thử sức với MAX88 qua các trò chơi như Tài Xỉu, Xóc đĩa và Cá cược bóng đá .
HEN88 là cổng game bài đổi thưởng hàng đầu tại Việt Nam, nổi bật với sự đa dạng trong các thể loại trò chơi. Từ slot game, xì dách, đến poker, mỗi game đều mang lại trải nghiệm độc đáo với đồ họa sắc nét và âm thanh sống động
MAX88 – Đẳng cấp cá cược online đến từ Anh Quốc. Thử sức với MAX88 qua các trò chơi như Tài Xỉu, Xóc đĩa và Cá cược bóng đá .
HUVIP88 – Cổng game đổi thưởng uy tín năm 2025 với hệ thống trò chơi phong phú từ game bài truyền thống đến các trò chơi mới lạ như Đua ngựa, Nổ hũ, Bắn cá, Rồng hổ, và Slot Games. Người chơi có thể trải nghiệm cảm giác hồi hộp với tài xỉu, xóc đĩa, bầu cua cùng nhiều tính năng độc đáo.
BOM86 là cổng game đổi thưởng đẳng cấp nhất hiện nay. Tại đây mọi người sẽ được trải nghiệm các game cá cược hấp dẫn như casino online , game bài và bắn cá.
See What Gas Central Heating Engineers Tricks
The Celebs Are Making Use Of gas Central heating engineers
Five Killer Quora Answers To Gas Boiler Engineer Near Me gas boiler engineer near me
What’s The Job Market For How Often Gas Safety Certificate Professionals?
how often gas safety certificate
Woah! I’m really digging the template/theme of this website.
It’s simple, yet effective. A lot of times it’s difficult to get that “perfect balance” between usability and appearance.
I must say that you’ve done a superb job with this.
Also, the blog loads super fast for me on Internet explorer.
Excellent Blog!
for the reason that here every material is quality based
9 Lessons Your Parents Teach You About Affordable SEO Company London Affordable Seo company
Why Gas Engineer Is More Difficult Than You Think Emergency gas engineer
su789 cổng game đổi thưởng uy tín, đa dạng, ưu đãi khủng đang chờ bạn. Nhận code tân thủ 100k cực hấp dẫn qua link chính thức https://su789.org/ hôm nay!
Five Killer Quora Answers On Gas Boiler Engineer Near Me Gas boiler engineer near me
SAM86 – Đẳng cấp và uy tín là các nhận xét từ người chơi đến cổng game đổi thưởng này. Người chơi hoàn toàn có thể yên tâm trải nghiệm các trò chơi các cược như xóc đĩa, tài xỉu, bắn cá và slot tại đây.
Guide To Corgi Gas Engineer Near Me: The Intermediate Guide In Corgi Gas Engineer Near Me corgi gas engineer near me (Dawn)
VB88 là nhà cái được đầu tư kỹ lưỡng, bảo mật cao và uy tín đến từ Dubai. Muôn vàn trò chơi cá cược thể thao như bóng đá , liên minh huyền thoại và các thể loại casino game bài, tài xỉu, xóc đĩa. Đi kèm là kho game nổ hũ và slot được thiết kế đẹp đẽ bắt mắt.
XO88 là nhà cái đẳng cấp từ Anh Quốc, cung cấp đa dạng trò chơi cá cược online như bóng đá, casino trực tuyến, xóc đĩa, tài xỉu và nổ hũ. Tham gia ngay để trải nghiệm!
Podem recomendar outros blogues/sites/fóruns que tratem dos mesmos temas?
5 Killer Quora Answers To Affordable Local
SEO Company affordable local Seo company
10 Websites To Help You To Become A Proficient In Gas Engineer Corgi Registered Gas Engineer
The Companies That Are The Least Well-Known To Follow In The Landlord Gas Safety
Certificate Industry landlord gas Safety certificate Cost
I’m impressed, I must say. Rarely do I come across a blog that’s both equally educative and amusing,
and without a doubt, you have hit the nail on the head.
The issue is something that not enough men and women are
speaking intelligently about. I am very happy I found
this during my search for something regarding this.
The Advanced Guide To Local SEO Marketing Agency link Building Agency Uk
If you’re a fan of action-packed fruit-slicing games, Slice Master is a title you don’t want to miss. With its latest upgrade available at Slicemaster.net
information.|My family members every time say that I am killing my time here
The Reason Why Boiler Repairs In Buckingham Will Be The Hottest Topic In 2024
Gas Safety Engineer Buckingham
Unexpected Business Strategies Helped Landlord Gas
Safety Certificate Newport Pagnell Succeed gas Safety engineers newport Pagnell
This is a topic that is close to my heart… Take care!
Exactly where are your contact details though?
9 Lessons Your Parents Teach You About Gas
Safety Checks Newport Pagnell Gas safety checks newport pagnell
You’ll Never Be Able To Figure Out This Gas Safe Engineer Newport Pagnell’s Tricks gas safe
Engineer Newport Pagnell (Bioimagingcore.Be)
10 Things That Your Family Teach You About Gas Safety Milton Keynes gas safety milton keynes [Deneen]
It’s great that you are getting ideas from this post as well as from our discussion made at this time.
Seven Issues About Juegos De Casino Online That You
Really Want… Badly CasinosEdge.pro
Are you ready to reel in the fun? The upgraded version of Tiny Fishing at TheTinyFishing.com takes your fishing experience to a whole new level. Dive into the exciting world of virtual fishing with enhanced features.
Esta página tem definitivamente toda a informação que eu queria sobre este assunto e não sabia a quem perguntar. Este é o meu primeiro comentário aqui, então eu só queria dar um rápido
You’ll Never Be Able To Figure Out This Gas Safe Engineer Newport Pagnell’s Benefits gas safe engineer Newport Pagnell
You’ll Be Unable To Guess Gas Safety Checks Milton Keynes’s Benefits gas safety checks milton keynes (Ingeborg)
5 Killer Quora Answers To Landlord Gas Safety Certificate Milton Keynes
Gas Safety Certificate Milton Keynes
13 Things About Newport Pagnell Heating Engineers You May Not Know gas engineers newport pagnell
Central Heating Engineers In Buckingham: 11 Things That You’re Failing To
Do Gas safety certificates Buckingham (Kenneth)
Hey there! Someone in my Myspace group shared this site with us so I came to look it over.
I’m definitely loving the information. I’m book-marking
and will be tweeting this to my followers! Superb blog and wonderful style and design.
10 Things That Your Family Taught You About Gas Safety Inspection Newport Pagnell gas safety inspection Newport Pagnell
Good article. I’m going through a few of these issues as well..
Děkuji|Ahoj všem, obsah, který je na této stránce k dispozici.
9 Lessons Your Parents Teach You About Landlord Gas Safety Certificate Milton Keynes Gas Safety Certificate Milton Keynes
What’s The Current Job Market For Boiler Gas Engineer Professionals?
boiler gas engineer – Emil –
10 Real Reasons People Dislike Gas Safety Certificate Price Gas Safety Certificate Price landlord gas safety certificate price (Danny)
You’ll Never Guess This Best SEO Software UK’s Secrets Seo software Uk
Hey There. I found your blog using msn. This is a really well written article.
I’ll be sure to bookmark it and return to read more of your
useful info. Thanks for the post. I will certainly comeback.
An outstanding share! I’ve just forwarded this onto a friend
who was doing a little homework on this. And he in fact bought me lunch because I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending some time to discuss this topic here on your
web page.
Why Gas Fire Service Engineers Near Me Is Your Next Big Obsession corgi gas safe engineers
You’ll Never Guess This Gas Safe Engineer Newport Pagnell’s Tricks gas safe engineer Newport Pagnell
IWIN 68 – Trang chủ tải IWIN68 club cho APK/IOS, cổng game đổi thưởng trực tuyến chính thức tặng code 99K tại iwin68-club.net. IWIN68 cổng game bài đổi thưởng trực tuyến hàng đầu tại Châu Á, với nhiều trò chơi hấp dẫn bầu cua, xóc đĩa, tài xỉu, casino, thể thao,…
What Is Gas Safety Milton Keynes And Why Is
Everyone Talking About It? gas Safety Certificate milton keynes
IWIN 68 – Trang chủ tải IWIN68 club cho APK/IOS, cổng game đổi thưởng trực tuyến chính thức tặng code 99K tại iwin68-club.net. IWIN68 cổng game bài đổi thưởng trực tuyến hàng đầu tại Châu Á, với nhiều trò chơi hấp dẫn bầu cua, xóc đĩa, tài xỉu, casino, thể thao,…
Podem recomendar outros blogues/sites/fóruns que tratem dos mesmos temas?
Five Killer Quora Answers To Gas Safety Certificate Newport
Pagnell Gas Safety Certificate Newport Pagnell
Great blog here! Also your web site loads up fast! What host are you using?
Can I get your affiliate link to your host? I wish my site loaded
up as fast as yours lol
Tak Hej der til alle, det indhold, der findes på denne
I all the time used to read piece of writing in news papers but now as
I am a user of internet thus from now I am using net for posts, thanks to web.
An impressive share! I’ve just forwarded this onto a
friend who has been doing a little research on this.
And he in fact ordered me dinner due to the fact that I found it for him…
lol. So allow me to reword this…. Thank YOU for the meal!!
But yeah, thanks for spending some time to discuss this subject here on your site.
vykřiknout a říct, že mě opravdu baví číst vaše příspěvky na blogu.
There’s definately a lot to know about this topic.
I like all the points you made.
I needed to thank you for this wonderful read!! I definitely loved every bit of it.
I have got you book marked to look at new stuff you post…
I go to see every day a few web sites and
information sites to read content, except this webpage offers feature
based writing.
88goals
duoc biet den nha mot nha cai uy tin hang dau khu vuc Chau A. Cac sanh ca cuoc cua nha cai nay duoc dau tu xay dung tren nen tang cong nghe hien dai. Chinh vi vay ma san choi nay duoc cong dong game thu danh gia chat luong dang choi nhat hien nay.
råb ud og sig, at jeg virkelig nyder at læse gennem dine blogindlæg.
10 Easy Steps To Start The Business Of Your Dream Local SEO
Services Company Business strategy
It’s amazing to pay a visit this site and reading the views of all colleagues
regarding this post, while I am also zealous of getting experience.
Hi, the whole thing is going well here and ofcourse every one is sharing facts,
that’s truly good, keep up writing.
A Step-By-Step Guide To Replacement Fiat 500 Key fiat Tipo key – liquidbush05.werite.net,
Thank you a lot for sharing this with all folks you actually recognise what you’re speaking approximately!
Bookmarked. Kindly also seek advice from my website =).
We will have a link trade agreement between us
I could not resist commenting. Well written!
Its like you read my mind! You seem to know a lot about this,
like you wrote the book in it or something. I think that you can do with a
few pics to drive the message home a bit, but other than that, this is magnificent blog.
A great read. I will certainly be back.
Replacing Panel In Upvc Door Tools To Ease Your Daily Life Replacing Panel In Upvc Door Trick That Should Be Used By Everyone Learn replacing panel In upvc door
Hello i am kavin, its my first occasion to commenting anywhere, when i
read this piece of writing i thought i could also create comment due to this brilliant post.
webside er virkelig bemærkelsesværdig for folks oplevelse, godt,
See What Misted Window Repair Near Me Tricks The Celebs Are Making Use Of misted window repair near me (Claude)
vip79 – game bài đại thần tài tải ngay phiên bản mới nhất 2025 tại vip79.reviews. Thử cược ngay, nhận thưởng khủng, dễ chơi, trúng lớn và nhận ngay code 179k!
Guide To Birth Injury Lawyer Near Me: The Intermediate Guide On Birth Injury Lawyer Near Me injury lawyer near me
Guide To Misty Windows Repair Near Me: The Intermediate Guide On Misty Windows Repair
Near Me Misty Windows Repair Near Me
aa
The 10 Scariest Things About Truck Wreck Attorney truck wreck attorney (Carla)
15 Best Accident Lawyer Near Me Bloggers You Should Follow best accident Lawyer near me
What You Must Forget About How To Improve Your Car Accident Lawyers top rated car Accident Lawyers
The Top Reasons Why People Succeed In The Best Car Accident Lawyers Industry lawyer for car
accidents (Leigh)
Why SEO Software For Small Business Is A Lot More
Risky Than You Think Search engine optimization software
Why Everyone Is Talking About Auto Accident Injury Attorney Today Lawyer For Car Accident Near Me
I’ll immediately snatch your rss as I can’t find your
email subscription link or e-newsletter service. Do you’ve any?
Kindly allow me recognize in order that I could subscribe.
Thanks.
5 Killer Quora Answers To Bi Fold Door Repair bi fold door repair, Shelli,
Hi there! I know this is kinda off topic but I was wondering if you knew where I could find a captcha plugin for my comment
form? I’m using the same blog platform as yours and I’m having problems finding one?
Thanks a lot!
Hey! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted
keywords but I’m not seeing very good results. If you know of any please share.
Thanks!
10 Train Accident Claim-Friendly Habits To Be Healthy construction truck accident lawyer
10 Unexpected Attorney Injury Accident Attorney Tips accident injury – Silas –
The Most Convincing Proof That You Need Train Derailment Lawyer truck driver Lawyers near me
Five Tools That Everyone Who Works In The Car
Locksmith Industry Should Be Making Use Of locked keys in Car locksmith
Guide To Lawyer Injury Accident: The Intermediate Guide The Steps To Lawyer
Injury Accident lawyer Injury
RR88 CASINO la mot nha cai co giay phep ca cuoc truc tuyen hop phap do Isle of Man va Khu kinh te Cagayan and Freeport cap.
) Znovu ho navštívím, protože jsem si ho poznamenal. Peníze a svoboda je nejlepší způsob, jak se změnit, ať jste bohatí a
The No. One Question That Everyone Working In Auto Accident Compensation Claim Needs To Know How To Answer Car Injury Attorneys Near Me
RR88 CASINO la mot nha cai co giay phep ca cuoc truc tuyen hop phap do Isle of Man va Khu kinh te Cagayan and Freeport cap.
Tak Hej der til alle, det indhold, der findes på denne
What’s The Reason You’re Failing At Auto Accident Lawyer For Hire Car accident And injury lawyers
Unexpected Business Strategies That Helped Truck Accident Lawsuits Achieve
Success semi truck Accident lawyers near me
10 Healthy Birth Injury Legal Process Habits attorneys injurys
(Concepcion)
Why People Don’t Care About Train Accident Settlement semi-truck accident lawyer
Hey very cool website!! Man .. Beautiful .. Amazing .. I’ll bookmark your blog and take the feeds also…I’m happy to find numerous useful info here in the post, we need work out more techniques in this regard, thanks for sharing. . . . . .
Ricwin la thuong hieu giai tri nhan duoc kha nhieu su quan tam thoi gian gan day. San choi duoc danh gia la dia chi de lam quen, mang lai nguon tai loc bat tan cho thanh vien. Ricwin88.com
nogensinde løbe ind i problemer med plagorisme eller krænkelse af ophavsretten? Mit websted har en masse unikt indhold, jeg har
Hello there! This post could not be written any better!
Reading this post reminds me of my old room mate! He always kept chatting about this.
I will forward this article to him. Fairly certain he will have a good read.
Many thanks for sharing!
Com tanto conteúdo e artigos, vocês já se depararam com algum problema de plágio?
The other day, while I was at work, my sister stole my iphone and tested to see if it can survive a thirty foot
drop, just so she can be a youtube sensation. My iPad is now destroyed and she has 83 views.
I know this is entirely off topic but I had to
share it with someone!
Xoilac TV phat song truc tiep bong da hom nay chat luong hinh anh cao Full HD, am thanh trung thuc suot 90Phut, khong giat lag. Xem bong da Xoi Lac TV cung binh luan vien Tieng Viet chuyen nghiep tai xoilacp.com
15 Twitter Accounts You Should Follow To Discover More About Birth Injury Advocate Attorneys injurys
If you desire to take a good deal from this piece
of writing then you have to apply such methods to
your won website.
reading this weblog’s post to be updated daily.
Attractive component of content. I simply stumbled upon your
website and in accession capital to assert that I get actually loved account your blog posts.
Anyway I will be subscribing for your augment
and even I fulfillment you get admission to consistently rapidly.
I’ll right away clutch your rss feed as I can not find your email subscription link or e-newsletter service.
Do you have any? Kindly let me realize in order that I could
subscribe. Thanks.
HDBET nha cai uy tin hang dau Viet Nam duoc thanh lap nam 2018 dat tru so chinh tai Dubai, hoat dong tren thi truong 18 quoc gia va vung lanh tho. HDBET.us la trang chu chinh thuc cua nha cai HDBET.COM, noi ban co the truy cap HDBET ma khong bi chan
Hi, I do think this is an excellent web site. I stumbledupon it ;
) I will return once again since I bookmarked it. Money and freedom is the best
way to change, may you be rich and continue to help other people.
) Vou voltar a visitá-lo uma vez que o marquei no livro. O dinheiro e a liberdade são a melhor forma de mudar, que sejas rico e continues a orientar os outros.
It’s Time To Upgrade Your Lovense Sex Machine Options cheapest sex machines – google.st
–
Wow, this piece of writing is good, my sister is analyzing these
things, so I am going to tell her.
Chính thức ra mắt thị trường cá cược vào năm 2021, Shbet gây ấn tượng với giao diện sắc nét với gam màu xanh biển đại diện cho sự trường thịnh kết hợp sắc trắng tinh khôi ngụ ý về sự mới lạ đã giúp nhà cái giữ chân hàng triệu cược thủ. shbet50.asia
Hello, i feel that i noticed you visited my blog thus i got here to return the choose?.I’m attempting
to find things to enhance my website!I assume its
good enough to use a few of your ideas!!
Remarkable! Its in fact remarkable piece of writing, I have got
much clear idea about from this post.
Sau 13 năm đi vào hoạt động, nhà cái 789Bet đã khẳng định được vị thế và sự khác biệt của mình. Địa chỉ cá cược trực tuyến chuyên nghiệp hàng đầu Châu Á kể trên được bet thủ biết đến từ năm 2011 và liên tục có những đổi mới, cải thiện đáng nể. 789bet.care
It contains fastidious material.|I think the admin of this website is actually working hard in favor of his site,
My developer is trying to persuade me to move to .net from PHP.
I have always disliked the idea because of the costs. But he’s tryiong none the less.
I’ve been using WordPress on various websites for about a year and am
nervous about switching to another platform. I have heard good things about blogengine.net.
Is there a way I can import all my wordpress content into it?
Any kind of help would be greatly appreciated!
Excellent post. I used to be checking constantly
this weblog and I am impressed! Extremely helpful information specially the closing section 🙂 I handle such information a lot.
I used to be seeking this certain info for a very lengthy time.
Thanks and best of luck.
789bet là Sân chơi công bằng, minh bạch, nhân văn kể trên giúp chúng ta cược thể thao, game bài đổi thưởng, bắn cá, slot, lô đề online, đá gà như ý. tại 789bett.asia
Good post! We will be linking to this great article on our
site. Keep up the good writing.
Trải nghiệm mượt mà như ý đã giúp SHBet giúp chúng ta được cá cược theo ý muốn đơn giản. Kho game khủng với nhiều trò cược như thể thao, xổ số, game bài đổi thưởng bắn cá, slot, lô đề online… shbet50.one
Giao diện màu Đỏ son kết hợp tone Đen huyền bí giúp 12Bet gây ấn tượng với người nhìn ngay từ giây đầu tiên. Địa chỉ cá cược trực tuyến chuyên nghiệp hàng đầu Châu Á kể trên đang cung cấp hàng loạt game khủng. 12bet.sarl
Hi, i think that i saw you visited my blog so i came to “return the favor”.I am attempting to find things to improve my
site!I suppose its ok to use some of your ideas!!
gruppe? Der er mange mennesker, som jeg tror virkelig ville
værdsætter dit indhold. Lad mig venligst vide det.
Hello there! This is my first visit to your blog!
We are a team of volunteers and starting a new project in a community in the same niche.
Your blog provided us useful information to work on.
You have done a extraordinary job!
What i don’t realize is in reality how you are no longer actually much more neatly-appreciated than you might be now.
You’re so intelligent. You already know thus considerably relating to this subject,
produced me personally imagine it from numerous numerous angles.
Its like women and men are not interested except it’s
something to do with Girl gaga! Your personal stuffs nice.
Always maintain it up!
Chính thức ra mắt thị trường cá cược vào năm 2021, Shbet gây ấn tượng với giao diện sắc nét với gam màu xanh biển đại diện cho sự trường thịnh kết hợp sắc trắng tinh khôi ngụ ý về sự mới lạ đã giúp nhà cái giữ chân hàng triệu cược thủ. shbet50.asia
Hi88 là website công ty giải trí chính thức của nhà cái hi88, bao gồm hệ thống game cá cược đa dạng đỉnh cao như cá độ thể thao, bóng đá, esport, đá gà, đua ngựa, game bài, slot game, nổ hũ và quay số keno, bingo, xổ số lô đề có tại hi88t.me
5 Reasons To Consider Being An Online Mesothelioma Asbestos Claim Business And 5
Reasons To Not mesothelioma lawsuits
Trải nghiệm mượt mà như ý đã giúp SHBet giúp chúng ta được cá cược theo ý muốn đơn giản. Kho game khủng với nhiều trò cược như thể thao, xổ số, game bài đổi thưởng bắn cá, slot, lô đề online… shbet50.one
vykřiknout a říct, že mě opravdu baví číst vaše příspěvky na blogu.
Don’t Buy Into These “Trends” Concerning Best Car Accident Lawyer
Near Me car wreck attorney (Nicole)
Wi88 duoc nhieu thanh vien yeu thich va danh gia cao trong gioi nha cai ca cuoc va game bai doi thuong. Neu ban dang tim kiem dia chi uy tin, hay lua chon ngay san choi nay ngay nhe! wi88.nl
O conteúdo existente nesta página é realmente notável para a experiência das pessoas,
The Companies That Are The Least Well-Known To Watch In The Best Bedside Cot Industry Cot for bedside
Fiquei muito feliz em descobrir este site. Preciso de agradecer pelo vosso tempo
I always emailed this website post page to all my contacts,
for the reason that if like to read it afterward my links will too.
What’s up i am kavin, its my first occasion to commenting anyplace, when i
read this post i thought i could also create comment
due to this sensible post.
Five Killer Quora Answers To GSA SER List gsa ser list
TDTC (Thiên Đường Trò Chơi) là website game trực tuyến uy tín nhất hiện nay, với các Game Bài, Thể Thao, Xổ Số, Bắn Cá, Tài Xỉu… tdtc.store
10 Quick Tips About Hiring Auto Accident Lawyers car crash attorney (Chandra)
188BET là sòng bạc trực tuyến thuộc liên minh OKVIP. 188BET cung cấp đa dạng sản phẩm cá cược như: casino, xổ số, bắn cá, đá gà, cá cược thể thao. 188bett.asia
ocenili váš obsah. Dejte mi prosím vědět.
Nhà cái 789bet là địa điểm cá cược online, sở hữu số lượng thành viên đông đảo. Để nắm rõ thông tin về nhà cái 789bet.promo mọi người hãy theo dõi bài viết sau.
Thanks very interesting blog!
188BET là sòng bạc trực tuyến thuộc liên minh OKVIP. 188BET cung cấp đa dạng sản phẩm cá cược như: xổ số, bắn cá, đá gà, cá cược thể thao.. 188bet0.pro
Nice post. I learn something new and challenging on sites
I stumbleupon on a daily basis. It will always be interesting
to read content from other writers and use a
little something from other sites.
Wow, wonderful weblog format! How long have you been running a
blog for? you make blogging glance easy. The full look of your site is wonderful,
as well as the content material!
188BET hiện đang cung cấp sản phẩm cá cược cho hàng trăm cược thủ mỗi ngày. Tạo ngay một tài khoản, nạp tiền và đặt cược tại đây chắc chắn bạn sẽ tạo cho mình niềm vui mỗi ngày. 188bet0.me
Mayclub là địa chỉ giải trí online uy tín mang đến trải nghiệm thú vị và hấp dẫn. Người chơi không chỉ tận hưởng sự đa dạng về thể loại mà còn được đảm bảo tính công bằng, minh bạch. mayclubs.com
Appreciation to my father who informed me concerning this website, this webpage
is really awesome.
Hey would you mind sharing which blog platform you’re working with?
I’m planning to start my own blog soon but I’m
having a difficult time choosing between BlogEngine/Wordpress/B2evolution and Drupal.
The reason I ask is because your design seems
different then most blogs and I’m looking for something unique.
P.S Apologies for being off-topic but I had to ask!
på grund af denne vidunderlige læsning !!! Jeg kunne bestemt virkelig godt lide hver eneste lille smule af det, og jeg
It’s not my first time to go to see this site, i am browsing
this web page dailly and obtain pleasant data from here all the time.
I am really enjoying the theme/design of your website. Do you ever run into any web browser compatibility issues? A few of my blog readers have complained about my website not operating correctly in Explorer but looks great in Chrome. Do you have any tips to help fix this issue?
Howdy! Do you use Twitter? I’d like to follow you if that would be ok.
I’m definitely enjoying your blog and look forward to new updates.
We are a gaggle of volunteers and opening a brand new scheme in our community.
Your site offered us with useful information to work on. You have done a formidable job and
our entire community will be grateful to you.
Simply wish to say your article is as astounding. The clarity
in your post is just nice and i could assume you are an expert on this subject.
Fine with your permission allow me to grab your feed
to keep up to date with forthcoming post. Thanks a million and please carry on the rewarding work.
Sweet blog! I found it while browsing on Yahoo News.
Do you have any suggestions on how to get listed
in Yahoo News? I’ve been trying for a while but
I never seem to get there! Thanks
Podem recomendar outros blogues/sites/fóruns que tratem dos mesmos temas?
I love what you guys are up too. This kind of clever work and exposure! Keep up the terrific works guys I’ve included you guys to our blogroll.
الاستمرار في توجيه الآخرين.|Ahoj, věřím, že je to vynikající blog. Narazil jsem na něj;
Great post. I was checking continuously this blog and I’m impressed!
Very useful information specially the last part 🙂 I care for such info a lot.
I was seeking this particular information for a very long time.
Thank you and best of luck.
I was recommended this blog by my cousin. I’m not sure whether this post is written by him
as nobody else know such detailed about my trouble. You’re wonderful!
Thanks!
Which Website To Research Mines Game Online Mines Game Online
With havin so much content and articles do you ever run into any problems of plagorism or copyright violation? My website has a lot of unique content I’ve either created myself or outsourced but it looks like a lot of it is popping it up all over the internet without my agreement. Do you know any methods to help reduce content from being stolen? I’d definitely appreciate it.
This will be a terrific website, will you be involved in doing an interview regarding just how you developed it? If so e-mail me!
Thanks a bunch for sharing this with all people you actually understand
what you’re speaking approximately! Bookmarked. Kindly also talk over with my website =).
We can have a link exchange arrangement among us
It is appropriate time to make a few plans for the
future and it’s time to be happy. I’ve read this put up and
if I may just I desire to suggest you some fascinating issues or advice.
Perhaps you could write subsequent articles referring to this article.
I desire to read more issues about it!
Thanks for sharing your info. I truly appreciate your efforts and I am waiting for your next post
thank you once again.
You’ll Be Unable To Guess Link Building Company’s Benefits link building company; Angeline,